When diagnosing Amyotrophic Lateral Sclerosis (ALS), healthcare providers rely on various clinical assessments to evaluate muscle weakness patterns. One significant diagnostic tool is the split hand test, which examines specific muscle weakness patterns in the hands that are characteristic of ALS. Understanding this test can help both medical professionals and patients recognize early signs of the condition.
The split hand phenomenon has become an increasingly important marker in ALS diagnosis, as it helps distinguish ALS from other neuromuscular conditions. This article explores how the test works, its significance in diagnosis, and its limitations.
What is the Split Hand Test?
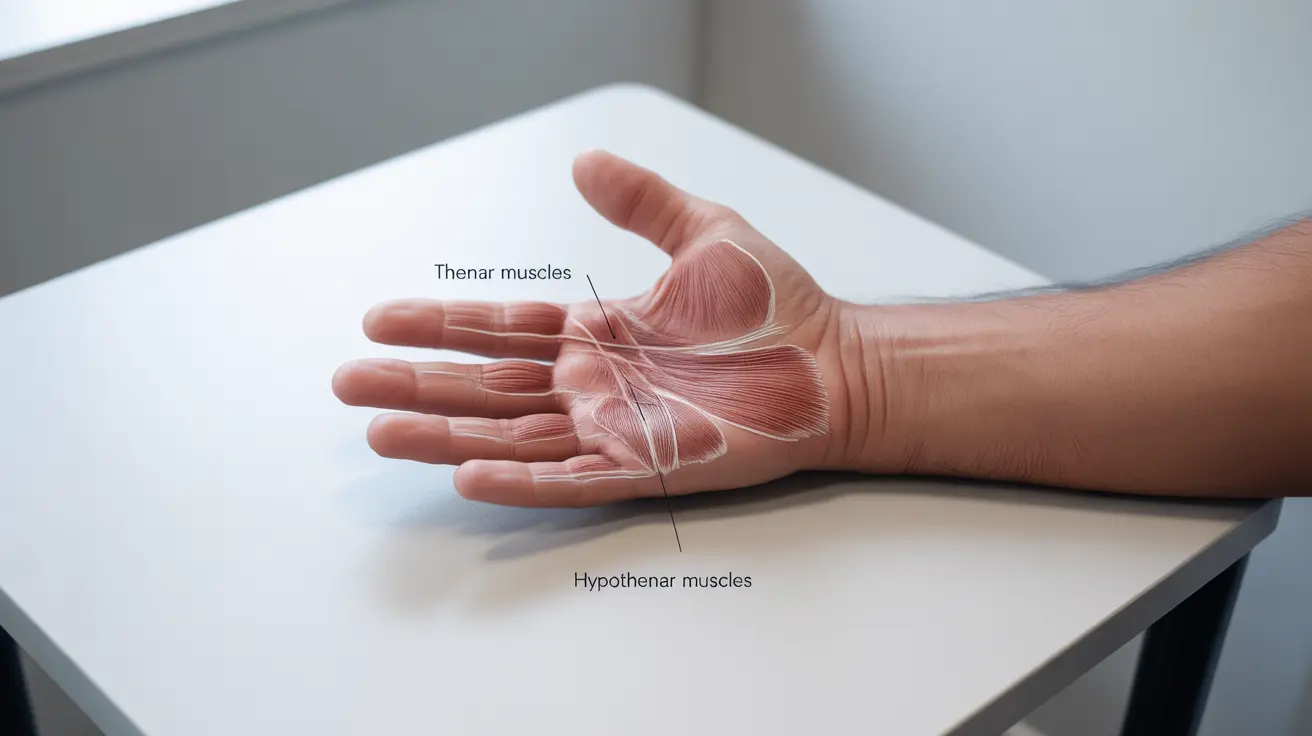
The split hand test evaluates the differential weakness between different muscle groups in the hand. Specifically, it measures the strength disparity between the thumb and pinky finger muscles. In ALS patients, there's typically more pronounced weakness in the thumb-side muscles (thenar) compared to the pinky-side muscles (hypothenar).
This distinctive pattern of muscle weakness is particularly valuable because it often appears early in the disease progression, sometimes before other classic ALS symptoms become apparent.
How the Split Hand Index is Measured
Medical professionals use several methods to measure the split hand index:
- Compound Muscle Action Potential (CMAP) recordings
- Manual muscle testing
- Hand grip dynamometer measurements
- Specialized neurophysiological testing
The most precise measurement involves comparing the CMAP amplitudes of specific hand muscles using nerve conduction studies. This provides objective data about muscle function and deterioration patterns.
Clinical Significance in ALS Diagnosis
The split hand test serves several important diagnostic purposes:
- Early detection of potential ALS symptoms
- Differentiation from other neurological conditions
- Monitoring disease progression
- Guiding treatment planning
However, it's crucial to understand that this test is just one piece of the diagnostic puzzle. Healthcare providers must consider it alongside other clinical findings and diagnostic tests.
Additional Diagnostic Considerations
While the split hand phenomenon is strongly associated with ALS, several other factors must be evaluated:
- Complete neurological examination
- Electromyography (EMG) studies
- Magnetic Resonance Imaging (MRI)
- Blood tests to rule out other conditions
- Medical history review
This comprehensive approach helps ensure accurate diagnosis and appropriate treatment planning.
Frequently Asked Questions
What is the split hand test and how does it relate to ALS diagnosis?
The split hand test examines the pattern of muscle weakness between different hand muscle groups, particularly comparing thumb-side muscles to pinky-side muscles. It's relevant to ALS diagnosis because this specific pattern of weakness is characteristic of the disease.
How is the split hand index measured and what does it reveal about hand muscle weakness in ALS?
The split hand index is measured through nerve conduction studies, manual muscle testing, and specialized equipment. It reveals a disproportionate weakness in thumb-controlling muscles compared to pinky muscles, which is typical in ALS.
Can the split hand test alone diagnose ALS, or does it need additional neurological evaluations?
The split hand test cannot diagnose ALS alone. While it's a valuable diagnostic tool, it must be combined with other neurological evaluations, EMG studies, and clinical assessments for a definitive ALS diagnosis.
What other conditions can cause a split hand pattern similar to ALS?
While the split hand pattern is strongly associated with ALS, similar patterns can occasionally occur in other conditions such as cervical radiculopathy, peripheral neuropathies, and certain muscle disorders. This is why comprehensive testing is essential.
How accurate is the split hand index test in distinguishing ALS from other neuromuscular disorders?
The split hand index test has shown high sensitivity and specificity for ALS when properly administered, but it's most accurate when considered alongside other diagnostic criteria. Its accuracy increases when combined with other clinical and neurophysiological findings.