Aqueous deficient dry eye is a specific type of dry eye syndrome where the lacrimal glands don't produce enough tears to keep your eyes properly lubricated. This condition can significantly impact your daily life, causing discomfort and potentially affecting your vision if left untreated. Understanding its causes, symptoms, and treatment options is crucial for managing this chronic condition effectively.
Unlike other forms of dry eye disease, aqueous deficient dry eye specifically relates to decreased tear production rather than increased tear evaporation or poor tear quality. This distinction makes it particularly important to receive an accurate diagnosis and appropriate treatment plan from an eye care professional.
Understanding Aqueous Deficient Dry Eye
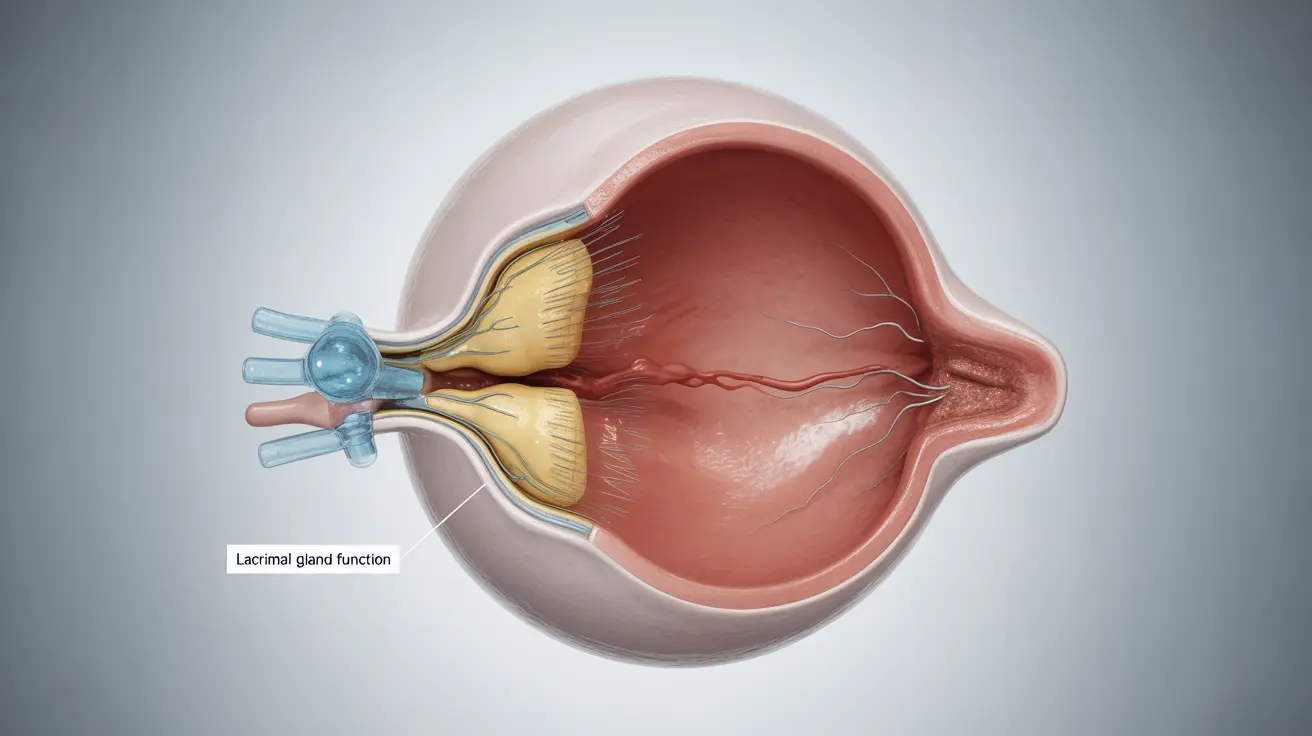
Aqueous deficient dry eye occurs when the lacrimal glands, which are responsible for producing the watery component of tears, fail to generate adequate moisture. This condition can be caused by various factors, including autoimmune disorders, aging, certain medications, and damage to the tear-producing glands.
The tear film consists of three layers: oil (lipid), water (aqueous), and mucin. In aqueous deficient dry eye, it's specifically the middle aqueous layer that's insufficient, leading to inadequate eye lubrication and protection.
Common Signs and Symptoms
Recognizing the symptoms of aqueous deficient dry eye is crucial for seeking timely treatment. Common indicators include:
- Persistent eye irritation
- Burning or stinging sensation
- Feeling of grittiness or foreign body sensation
- Difficulty wearing contact lenses
- Blurred vision that may improve with blinking
- Eye fatigue, especially during digital device use
- Sensitivity to light
Diagnostic Process
Eye care professionals use several specialized tests to diagnose aqueous deficient dry eye and distinguish it from other forms of dry eye disease. These typically include:
- Schirmer's test to measure tear production
- Tear break-up time (TBUT) assessment
- Corneal staining to check for surface damage
- Detailed examination of the tear film and glands
- Review of medical history and medications
Treatment Approaches
Managing aqueous deficient dry eye often requires a multi-faceted approach. Treatment options may include:
Medical Interventions
- Prescription eye drops to increase tear production
- Punctal plugs to retain natural tears
- Anti-inflammatory medications
- Autologous serum drops in severe cases
Supportive Measures
- Artificial tears and lubricating eye drops
- Proper eyelid hygiene
- Omega-3 fatty acid supplements
- Moisture chamber glasses or goggles
Lifestyle and Environmental Modifications
Several lifestyle changes can help manage symptoms and improve comfort:
- Maintaining proper humidity levels in living spaces
- Taking regular breaks during computer use
- Staying well-hydrated
- Protecting eyes from wind and harsh environments
- Avoiding smoke and other irritants
- Using air filters to reduce airborne particles
Frequently Asked Questions
What causes aqueous deficient dry eye and how is it different from other types of dry eye? Aqueous deficient dry eye is caused by insufficient tear production from the lacrimal glands, unlike other types of dry eye that may result from excessive evaporation or poor tear quality. It's often associated with autoimmune conditions, aging, or medication side effects.
What are the common symptoms of aqueous deficient dry eye that I should watch for? Key symptoms include persistent eye irritation, burning sensations, feeling of grittiness, difficulty wearing contact lenses, blurred vision that improves with blinking, and increased light sensitivity.
How is aqueous deficient dry eye diagnosed by an eye care professional? Diagnosis involves specialized tests including Schirmer's test, tear break-up time assessment, corneal staining, and comprehensive examination of the tear film and glands, along with a review of medical history.
What treatment options are available to increase tear production for aqueous deficient dry eye? Treatment options include prescription eye drops to stimulate tear production, punctal plugs, anti-inflammatory medications, artificial tears, and in some cases, autologous serum drops. The treatment plan is typically customized based on severity and individual needs.
Can lifestyle changes or environmental factors help prevent or reduce symptoms of aqueous deficient dry eye? Yes, lifestyle modifications can help manage symptoms. These include maintaining proper humidity levels, taking regular screen breaks, staying hydrated, protecting eyes from harsh environments, and avoiding irritants like smoke. Using air filters and maintaining good eye hygiene can also be beneficial.