An atherectomy is a specialized medical procedure designed to remove plaque buildup from blood vessels, particularly in cases where arterial blockages threaten heart health. This minimally invasive treatment option has become increasingly important in modern cardiovascular medicine, offering hope to patients with severe arterial disease.
Understanding what an atherectomy involves, its benefits, and what to expect can help patients make informed decisions about their cardiovascular care. This comprehensive guide explores the procedure in detail, including its purposes, techniques, and recovery process.
What Is an Atherectomy?
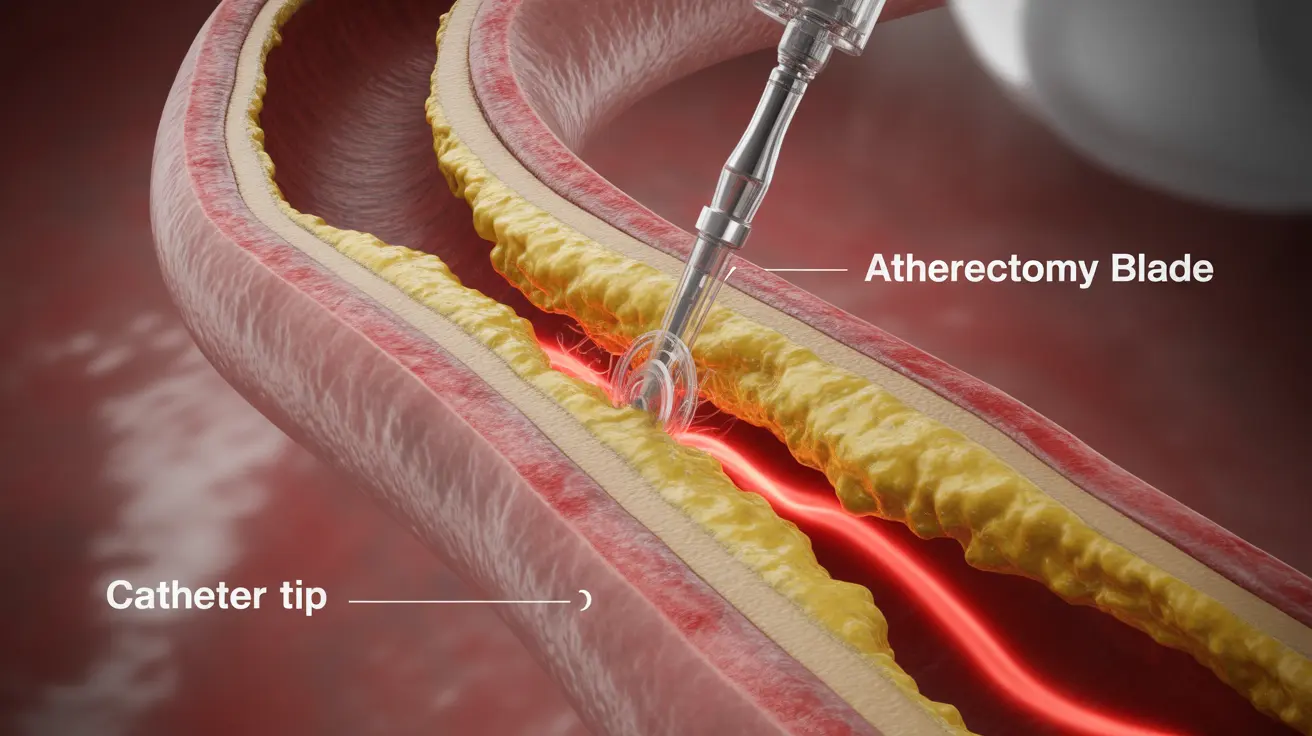
An atherectomy is a catheter-based procedure that uses specialized tools to remove atherosclerotic plaque from blood vessels. Unlike angioplasty, which compresses plaque against vessel walls, atherectomy actually cuts away and removes the problematic buildup, helping to restore proper blood flow.
Types of Atherectomy Procedures
There are several different approaches to performing an atherectomy, each suited to specific situations:
- Directional atherectomy
- Rotational atherectomy
- Orbital atherectomy
- Laser atherectomy
The Procedure Process
Before the Procedure
Preparation for an atherectomy involves several important steps:
- Medical evaluation and testing
- Review of current medications
- Fasting for several hours before the procedure
- Arrangement of transportation home
- Discussion of potential risks with healthcare providers
During the Procedure
The atherectomy procedure typically takes between one to two hours. Patients receive local anesthesia and possibly mild sedation. The doctor makes a small incision, usually in the groin area, to insert the catheter that will carry the atherectomy device to the blocked artery.
Recovery and Aftercare
After the procedure, patients typically:
- Remain in hospital for monitoring (usually 6-24 hours)
- Must lie flat for several hours to prevent bleeding
- Receive specific instructions about activity limitations
- Schedule follow-up appointments for monitoring progress
Benefits and Risks
Advantages
Atherectomy offers several significant benefits:
- Minimally invasive approach
- Often immediate improvement in blood flow
- Can treat heavily calcified plaques
- May reduce the need for stenting in some cases
Potential Complications
While generally safe, patients should be aware of possible risks:
- Bleeding at the insertion site
- Blood vessel damage
- Blood clots
- Restenosis (re-narrowing of the artery)
- Infection
Frequently Asked Questions
What is an atherectomy procedure and how does it help treat blocked arteries?
An atherectomy is a minimally invasive procedure that uses specialized catheter-based tools to remove plaque buildup from blocked arteries. The procedure helps restore proper blood flow by physically removing the blockage rather than just compressing it against the vessel wall.
What are the risks and potential complications of undergoing an atherectomy?
The main risks include bleeding, blood vessel damage, blood clots, infection, and the possibility of restenosis. However, serious complications are relatively rare when performed by experienced physicians in appropriate medical facilities.
How does atherectomy compare to angioplasty for treating arterial plaque buildup?
While angioplasty compresses plaque against the vessel wall, atherectomy actually removes the plaque from the artery. This makes atherectomy particularly useful for treating heavily calcified plaques or areas where stenting might be challenging.
What should I expect before, during, and after an atherectomy procedure?
Before the procedure, you'll undergo medical evaluation and receive specific preparation instructions. During the procedure, you'll receive local anesthesia and mild sedation. After the procedure, you'll need to lie flat for several hours and may stay in the hospital for monitoring before returning home.
Who is a good candidate for atherectomy treatment and when is it recommended?
Atherectomy is typically recommended for patients with significant plaque buildup who haven't responded well to medication or lifestyle changes. It's particularly suitable for those with heavily calcified plaques, complex lesions, or in locations where stenting might be difficult.