When dealing with chronic back pain and stiffness, understanding the specific condition affecting you is crucial for proper treatment and management. Two closely related inflammatory conditions often cause confusion among patients and even healthcare providers: axial spondyloarthritis and ankylosing spondylitis. While these conditions share many similarities, they represent different stages or presentations of the same disease spectrum.
This comprehensive guide will help you understand the key differences between axial spondyloarthritis and ankylosing spondylitis, their diagnostic processes, symptoms, and treatment approaches. Whether you've recently received a diagnosis or are seeking clarity about these conditions, this information will provide valuable insights into managing your spinal health effectively.
Understanding the Disease Spectrum
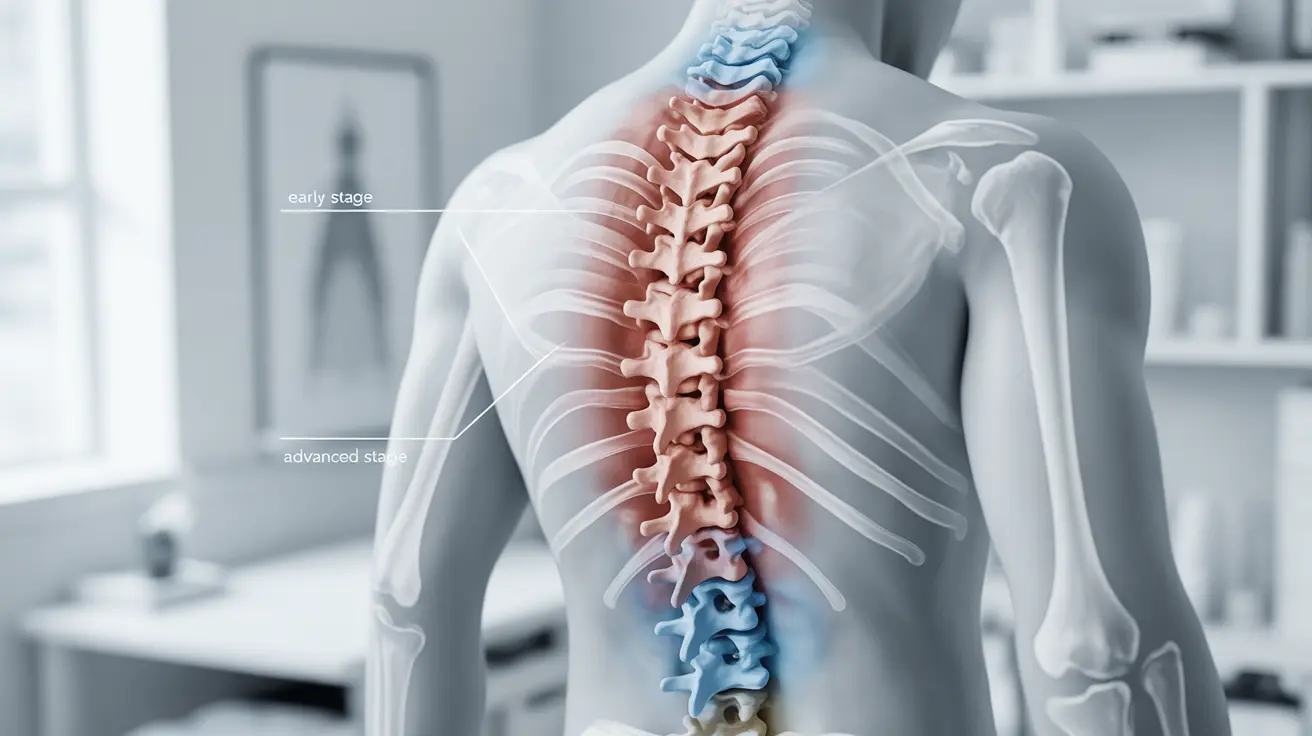
Axial spondyloarthritis represents a broader category of inflammatory diseases that primarily affect the spine and sacroiliac joints. This umbrella term encompasses two main subtypes based on whether structural damage is visible on X-rays. The classification system helps healthcare providers better understand disease progression and tailor treatment approaches accordingly.
Ankylosing spondylitis, historically considered a separate condition, is now understood as the more advanced form of axial spondyloarthritis. This reclassification occurred as medical understanding evolved, recognizing that these conditions exist on a continuous spectrum rather than as distinct diseases. The key distinguishing factor lies in the presence or absence of structural changes visible through imaging studies.
Non-Radiographic vs Radiographic Axial Spondyloarthritis
The primary distinction between axial spondyloarthritis and ankylosing spondylitis centers on radiographic evidence of structural damage. Non-radiographic axial spondyloarthritis occurs when patients experience characteristic symptoms and show inflammation on MRI scans, but X-rays do not yet reveal structural changes in the sacroiliac joints or spine.
In contrast, ankylosing spondylitis represents the radiographic form of axial spondyloarthritis, where X-rays clearly show structural damage such as erosions, sclerosis, or fusion of joints. This progression from non-radiographic to radiographic disease typically occurs over several years, though not all patients with non-radiographic disease will progress to the radiographic stage.
Diagnostic Approaches and Challenges
Diagnosing axial spondyloarthritis versus ankylosing spondylitis requires a comprehensive approach combining clinical assessment, laboratory tests, and imaging studies. Healthcare providers rely on established classification criteria that consider symptoms, family history, response to anti-inflammatory medications, and specific genetic markers like HLA-B27.
The diagnostic process often begins with a thorough medical history focusing on the pattern and characteristics of back pain. Inflammatory back pain, which improves with movement and worsens with rest, serves as a key distinguishing feature from mechanical back pain. Blood tests may reveal elevated inflammatory markers and the presence of HLA-B27, though this genetic marker alone is not diagnostic.
Advanced imaging plays a crucial role in differentiation. While X-rays may appear normal in early-stage disease, MRI scans can detect bone marrow edema and inflammation in the sacroiliac joints and spine. This imaging capability has revolutionized early diagnosis, allowing healthcare providers to identify and treat the condition before permanent structural damage occurs.
Symptom Patterns and Disease Manifestations
Both conditions share remarkably similar symptom profiles, which explains why they're now considered part of the same disease spectrum. The hallmark symptom involves chronic inflammatory back pain that typically begins before age 45 and persists for more than three months. This pain characteristically improves with movement and exercise while worsening during periods of inactivity.
Morning stiffness represents another common feature, often lasting more than 30 minutes and sometimes several hours. Patients frequently report difficulty getting out of bed or significant stiffness after sitting for extended periods. The pain and stiffness typically respond well to non-steroidal anti-inflammatory drugs (NSAIDs), providing both diagnostic and therapeutic value.
Beyond spinal symptoms, both conditions may involve peripheral manifestations including arthritis in other joints, particularly in the hips, shoulders, and peripheral joints of the arms and legs. Extra-articular features such as eye inflammation (uveitis), inflammatory bowel disease, and psoriasis can also occur in both forms of the condition.
Treatment Strategies and Management
Treatment approaches for axial spondyloarthritis and ankylosing spondylitis are remarkably similar, focusing on reducing inflammation, managing pain, and maintaining spinal mobility. The therapeutic strategy emphasizes early intervention to prevent or slow structural damage progression while maintaining quality of life.
First-line treatment typically involves NSAIDs, which effectively reduce inflammation and pain in most patients. Regular exercise and physical therapy play equally important roles, helping maintain spinal flexibility and prevent deformity. Specific exercises targeting posture, breathing, and spinal extension are particularly beneficial.
For patients who don't respond adequately to conventional therapy, biologic medications targeting specific inflammatory pathways have revolutionized treatment outcomes. TNF inhibitors and IL-17 inhibitors can significantly reduce inflammation, improve symptoms, and potentially slow disease progression in both non-radiographic and radiographic forms of the condition.
Disease Progression and Prognosis
Understanding disease progression helps patients and healthcare providers make informed treatment decisions. Studies suggest that approximately 10-20% of patients with non-radiographic axial spondyloarthritis will develop radiographic changes over a decade. However, this progression is not inevitable, and early treatment may help prevent or delay structural damage.
Several factors influence disease progression, including male gender, elevated inflammatory markers, presence of HLA-B27, and younger age at symptom onset. Regular monitoring through clinical assessments and imaging studies helps track disease activity and adjust treatment strategies accordingly.
The prognosis for both conditions has improved significantly with modern treatment approaches. Early diagnosis and appropriate therapy can help most patients maintain normal or near-normal function while preventing the severe spinal deformity historically associated with these conditions.
Frequently Asked Questions
What is the difference between axial spondyloarthritis and ankylosing spondylitis?
Axial spondyloarthritis is an umbrella term that includes two subtypes: non-radiographic axial spondyloarthritis and radiographic axial spondyloarthritis (also known as ankylosing spondylitis). The main difference lies in whether structural damage is visible on X-rays. Non-radiographic disease shows inflammation on MRI but no structural changes on X-rays, while ankylosing spondylitis demonstrates clear structural damage visible on X-ray imaging.
How is non-radiographic axial spondyloarthritis diagnosed compared to ankylosing spondylitis?
Both conditions use similar diagnostic criteria focusing on inflammatory back pain symptoms, family history, HLA-B27 testing, and response to NSAIDs. The key difference is in imaging: non-radiographic axial spondyloarthritis relies primarily on MRI evidence of inflammation in the absence of X-ray changes, while ankylosing spondylitis diagnosis requires visible structural damage on X-rays of the sacroiliac joints or spine.
What are the common symptoms of axial spondyloarthritis and how do they compare to ankylosing spondylitis?
The symptoms are virtually identical between both conditions, including chronic inflammatory back pain that improves with movement, morning stiffness lasting more than 30 minutes, pain that responds to NSAIDs, and potential peripheral joint involvement. Both may also present with extra-articular features like eye inflammation or inflammatory bowel disease. The symptom similarity reflects their position on the same disease spectrum.
What treatment options are available for axial spondyloarthritis and ankylosing spondylitis?
Treatment approaches are nearly identical for both conditions, emphasizing NSAIDs as first-line therapy, regular exercise and physical therapy, and biologic medications for patients with inadequate response to conventional treatment. The goal is reducing inflammation, managing pain, and maintaining spinal mobility regardless of whether structural damage is present on X-rays.
Can non-radiographic axial spondyloarthritis progress to ankylosing spondylitis over time?
Yes, some patients with non-radiographic axial spondyloarthritis may develop structural changes visible on X-rays over time, progressing to what is classified as ankylosing spondylitis. However, this progression occurs in only about 10-20% of patients over a decade and is not inevitable. Early treatment may help prevent or delay this progression, emphasizing the importance of proper diagnosis and management.