Bladder prolapse, also known as cystocele, is a condition that affects many women, particularly after childbirth or during menopause. Understanding the symptoms and available treatments is crucial for maintaining quality of life and seeking appropriate medical care. This comprehensive guide will help you recognize the signs and explore various management options.
Understanding Bladder Prolapse and Its Impact
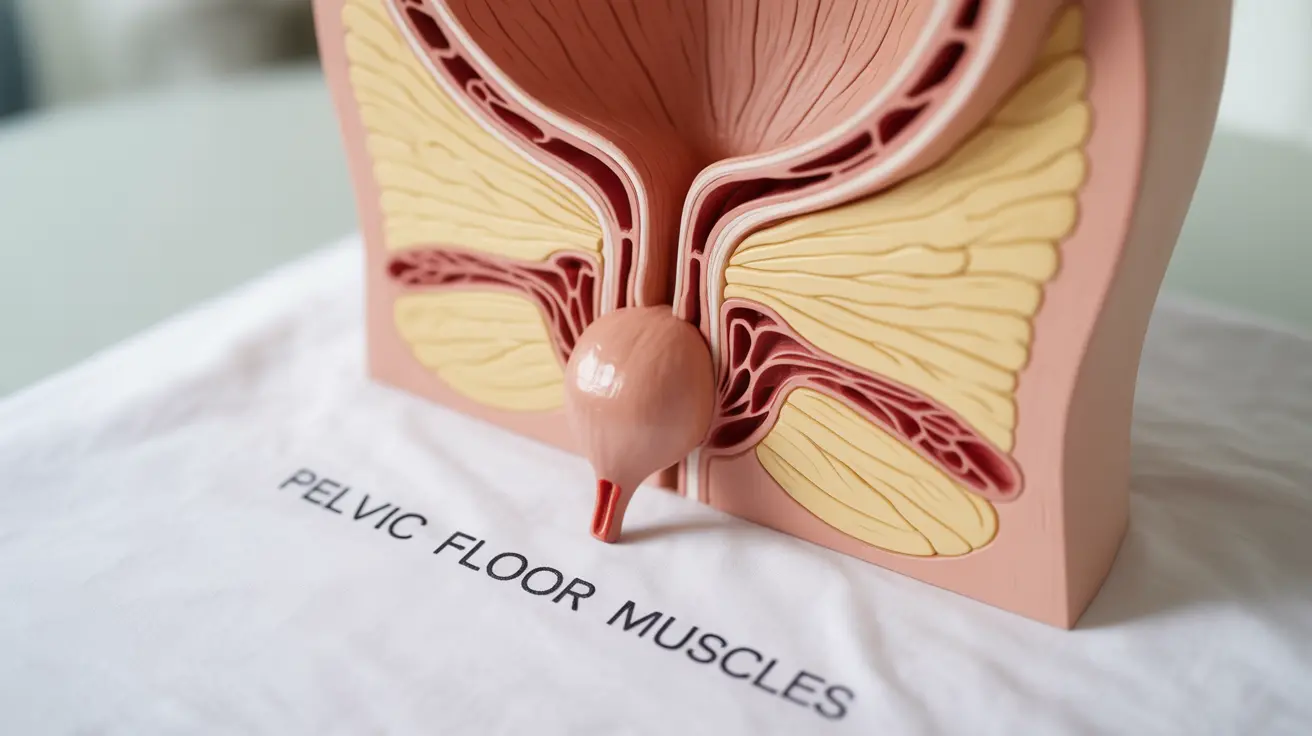
Bladder prolapse occurs when weakened pelvic floor muscles allow the bladder to drop from its normal position and push against the vaginal wall. This condition can significantly impact daily activities and comfort, but with proper understanding and treatment, many women can find relief from their symptoms.
Common Signs and Symptoms to Watch For
Recognizing bladder prolapse symptoms early can lead to more effective treatment outcomes. The most common indicators include:
- Feeling of pressure or fullness in the vaginal area
- A visible bulge at the vaginal opening
- Difficulty starting urination or fully emptying the bladder
- Frequent urinary tract infections
- Discomfort during physical activity
- Pain or pressure during intercourse
Diagnostic Process and Medical Evaluation
Healthcare providers use several methods to diagnose bladder prolapse accurately:
Physical Examination
Your doctor will perform a thorough pelvic examination to assess the extent of the prolapse and identify any additional pelvic floor issues.
Diagnostic Tests
Additional tests may include:
- Bladder function tests (urodynamics)
- Imaging studies such as ultrasound or MRI
- Voiding diary assessment
- Post-void residual measurement
Non-Surgical Treatment Options
Many women can manage their bladder prolapse symptoms through conservative treatments:
Pelvic Floor Exercises
Kegel exercises and other pelvic floor strengthening techniques can help support the bladder and improve symptoms.
Pessary Device
A removable device inserted into the vagina can provide support to the bladder and reduce prolapse symptoms.
Lifestyle Modifications
Simple changes can make a significant difference:
- Maintaining a healthy weight
- Avoiding heavy lifting
- Managing chronic cough
- Regular exercise with appropriate modifications
Surgical Intervention and Recovery
When conservative treatments aren't sufficient, surgical options may be considered. Modern surgical techniques include:
- Transvaginal repair
- Laparoscopic procedures
- Mesh reinforcement (in specific cases)
- Robotic-assisted surgery
Prevention and Long-term Management
Taking proactive steps can help prevent worsening of bladder prolapse:
- Regular pelvic floor exercises
- Maintaining good posture
- Proper lifting techniques
- Regular follow-up with healthcare providers
Frequently Asked Questions
What are the most common symptoms of bladder prolapse that I should watch for? The most common symptoms include a feeling of pressure in the vaginal area, difficulty with urination, a visible bulge in the vagina, lower back pain, and discomfort during physical activities or intercourse.
How is bladder prolapse diagnosed and what tests are usually involved? Diagnosis typically involves a detailed physical examination, including a pelvic exam. Your doctor may also order urodynamic testing, imaging studies like ultrasound or MRI, and ask you to keep a voiding diary.
What non-surgical treatments are available to manage bladder prolapse symptoms? Non-surgical treatments include pelvic floor exercises, pessary devices, lifestyle modifications, and weight management. Physical therapy specifically targeting the pelvic floor muscles can also be very effective.
When is surgery recommended for bladder prolapse, and what does the procedure involve? Surgery is typically recommended when conservative treatments fail to provide relief or when the prolapse significantly impacts quality of life. Procedures may include transvaginal repair, laparoscopic surgery, or mesh reinforcement, depending on individual circumstances.
What lifestyle changes can help prevent bladder prolapse or reduce its symptoms? Key lifestyle changes include maintaining a healthy weight, avoiding heavy lifting, practicing proper posture, performing regular pelvic floor exercises, and managing conditions that cause chronic coughing or straining.