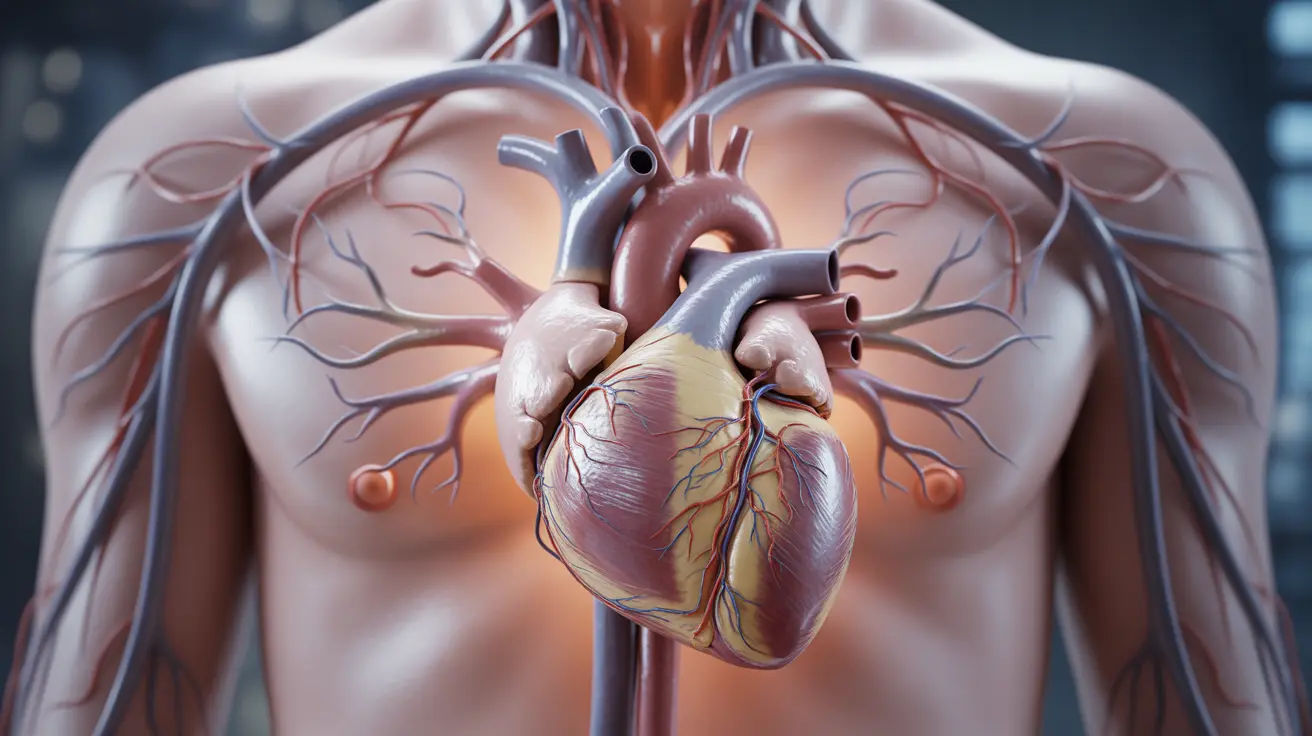
Many people discover that their blood pressure readings spike during nighttime hours, even when their daytime measurements appear normal. This phenomenon, known as nocturnal hypertension, affects a significant portion of the population and can be more concerning than elevated daytime readings. Understanding why your blood pressure might increase at night is crucial for maintaining optimal cardiovascular health.
Nighttime blood pressure elevation represents a complex medical issue that involves multiple physiological systems working differently during sleep cycles. While most people expect their blood pressure to naturally decrease during rest periods, various factors can disrupt this normal pattern, leading to potentially serious health implications.
Understanding Normal Blood Pressure Patterns
Under normal circumstances, blood pressure follows a predictable daily rhythm called the circadian pattern. During healthy sleep, blood pressure typically drops by 10-20% compared to daytime levels, a phenomenon medical professionals call "dipping." This natural decline allows your cardiovascular system to rest and recover from the day's activities.
When this normal dipping pattern doesn't occur, or when blood pressure actually increases at night, it indicates an underlying disruption in your body's natural regulatory mechanisms. This non-dipping or reverse-dipping pattern can place additional strain on your heart, blood vessels, and organs during what should be a restorative period.
Primary Causes of Nighttime Blood Pressure Spikes
Sleep-Related Disorders
Sleep apnea stands as one of the most common culprits behind nighttime blood pressure elevation. When breathing repeatedly stops and starts during sleep, oxygen levels drop, triggering stress responses that cause blood pressure to surge. These episodes can occur dozens or even hundreds of times per night, creating sustained pressure on the cardiovascular system.
Poor sleep quality, frequent awakenings, and sleep deprivation can also contribute to nighttime hypertension by disrupting the body's natural hormone production and stress response systems.
Medications and Timing
Certain medications can interfere with normal blood pressure patterns, particularly when taken at inappropriate times. Some blood pressure medications work more effectively when taken in the evening, while others may cause nighttime spikes if their timing isn't optimized.
Additionally, medications for other conditions, such as decongestants, pain relievers, and antidepressants, can contribute to elevated nighttime blood pressure as side effects.
Lifestyle and Dietary Factors
Evening habits significantly impact nighttime blood pressure patterns. Consuming large meals, alcohol, or caffeine close to bedtime can interfere with the body's natural preparation for sleep and rest. High sodium intake throughout the day can also contribute to fluid retention and elevated pressure during nighttime hours.
Physical inactivity during the day may prevent the natural fatigue that helps blood pressure drop at night, while excessive stress and anxiety can keep the body in a heightened state of alertness even during sleep.
Symptoms and Warning Signs
Recognizing nighttime hypertension can be challenging since many people are asleep when symptoms occur. However, certain warning signs may indicate elevated nighttime blood pressure, including morning headaches, dizziness upon waking, night sweats, and frequent urination during sleep hours.
Some individuals may experience chest discomfort, palpitations, or shortness of breath during the night. Persistent fatigue despite adequate sleep time can also signal that your cardiovascular system isn't getting proper rest due to elevated pressure.
It's important to note that many people with nighttime hypertension experience no obvious symptoms, making regular monitoring crucial for early detection and management.
Health Risks and Complications
Nighttime blood pressure elevation carries significant health risks that may exceed those associated with daytime hypertension. Research indicates that nocturnal hypertension increases the risk of cardiovascular events, including heart attacks, strokes, and heart failure, more dramatically than elevated daytime readings alone.
The continuous strain on blood vessels during what should be a recovery period can accelerate the development of atherosclerosis, kidney damage, and other organ complications. The lack of natural blood pressure dipping also prevents the cardiovascular system from experiencing necessary periods of reduced workload.
Natural Management Strategies
Several lifestyle modifications can help reduce nighttime blood pressure spikes naturally. Establishing a consistent sleep schedule supports your body's circadian rhythms, while creating a relaxing bedtime routine can help transition your body into rest mode more effectively.
Dietary adjustments play a crucial role in managing nighttime hypertension. Reducing sodium intake, avoiding large meals within three hours of bedtime, and limiting alcohol and caffeine consumption can significantly impact nighttime pressure patterns.
Regular physical activity during appropriate daytime hours helps promote natural fatigue and supports healthy blood pressure patterns. However, vigorous exercise should be avoided close to bedtime as it can have stimulating effects.
Stress management techniques, including meditation, deep breathing exercises, and progressive muscle relaxation, can help calm the nervous system and prepare the body for restorative sleep.
Diagnosis and Medical Evaluation
Diagnosing nighttime hypertension typically requires 24-hour ambulatory blood pressure monitoring, which provides continuous readings throughout day and night cycles. This comprehensive monitoring reveals patterns that standard office measurements might miss.
Home blood pressure monitoring can also provide valuable information, especially when measurements are taken at consistent times before bed and upon waking. Keeping detailed logs of readings, along with notes about sleep quality, medications, and lifestyle factors, helps healthcare providers identify patterns and potential triggers.
Sleep studies may be recommended if sleep apnea is suspected as an underlying cause, while additional tests might evaluate kidney function, hormone levels, and other factors that could contribute to nocturnal hypertension.
Treatment Approaches
Treatment for nighttime blood pressure elevation often involves a combination of medication adjustments and lifestyle modifications. Healthcare providers may recommend taking certain blood pressure medications in the evening rather than morning to provide better nighttime control.
Addressing underlying sleep disorders, particularly sleep apnea, can dramatically improve nighttime blood pressure patterns. Treatment with continuous positive airway pressure (CPAP) devices often leads to significant improvements in nocturnal hypertension.
For some individuals, specialized medications that target nighttime blood pressure specifically may be prescribed, while others benefit from adjustments to existing medication timing and dosages.
Frequently Asked Questions
Why does my blood pressure go up at night even if it's normal during the day?
Nighttime blood pressure elevation can occur due to several factors including sleep disorders like sleep apnea, medication timing issues, late evening meals, alcohol consumption, stress, or underlying medical conditions. Your body's natural circadian rhythm may be disrupted, preventing the normal 10-20% drop in blood pressure that should occur during sleep. This pattern, called non-dipping or reverse-dipping, requires medical evaluation to identify and address the underlying causes.
What are the symptoms of high blood pressure at night?
Symptoms of nighttime high blood pressure may include morning headaches, dizziness upon waking, night sweats, frequent nighttime urination, chest discomfort, palpitations, shortness of breath during sleep, and persistent fatigue despite adequate sleep time. However, many people experience no obvious symptoms, making regular blood pressure monitoring essential for detection. If you notice any of these symptoms consistently, consult your healthcare provider for proper evaluation.
How can I lower my blood pressure at night naturally?
Natural approaches to reduce nighttime blood pressure include maintaining a consistent sleep schedule, avoiding large meals, alcohol, and caffeine within 3 hours of bedtime, reducing daily sodium intake, practicing stress-reduction techniques like meditation or deep breathing, engaging in regular daytime physical activity, creating a relaxing bedtime routine, and ensuring your sleep environment is cool, dark, and quiet. Weight management and treating sleep disorders like sleep apnea are also crucial for natural nighttime blood pressure control.
What causes nighttime blood pressure spikes and how is it diagnosed?
Nighttime blood pressure spikes can be caused by sleep apnea, poor sleep quality, late-night eating or drinking, certain medications, chronic stress, kidney problems, or hormonal imbalances. Diagnosis typically involves 24-hour ambulatory blood pressure monitoring, which tracks your blood pressure continuously throughout day and night cycles. Home monitoring with detailed logs, sleep studies, and additional medical tests may also be used to identify underlying causes and develop appropriate treatment strategies.
Is high blood pressure at night more dangerous than during the day?
Research suggests that nighttime high blood pressure may actually be more dangerous than elevated daytime readings. Nocturnal hypertension is associated with higher risks of heart attacks, strokes, heart failure, and organ damage because it prevents your cardiovascular system from experiencing the natural rest period it needs. The continuous strain during sleep hours can accelerate blood vessel damage and increase cardiovascular complications more significantly than daytime hypertension alone, making proper diagnosis and treatment particularly important.