Finding blood in your stool, especially when experiencing constipation, can be alarming. While this combination of symptoms often has benign causes, understanding the underlying reasons and knowing when to seek medical attention is crucial for your health and peace of mind.
This comprehensive guide will help you understand the connection between constipation and blood in stool, identify common causes, and learn about appropriate treatment options and warning signs that require immediate medical attention.
Common Causes of Blood in Stool During Constipation
When constipation leads to blood in stool, several common conditions may be responsible:
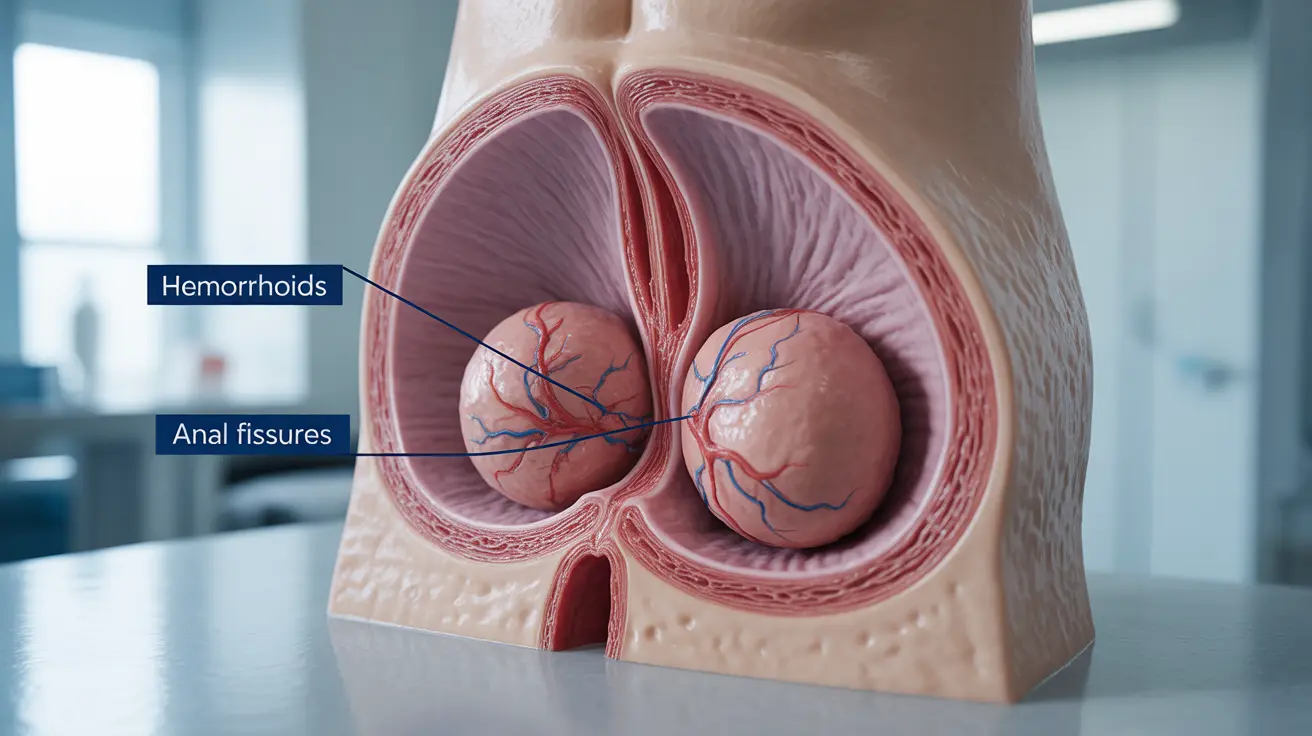
Hemorrhoids
Hemorrhoids are swollen blood vessels in the anal area that commonly develop due to straining during bowel movements. These can become irritated and bleed, especially when passing hard stools during constipation. The blood from hemorrhoids typically appears bright red and may be noticed on toilet paper or in the bowl.
Anal Fissures
Constipation often leads to anal fissures - small tears in the anal tissue that occur when passing large or hard stools. These tears can cause sharp pain during bowel movements and result in bright red bleeding that you might notice on toilet paper or in the toilet bowl.
Identifying the Source of Bleeding
Understanding the characteristics of the bleeding can help determine its likely cause:
- Bright red blood on toilet paper or in the bowl typically indicates hemorrhoids or anal fissures
- Darker blood mixed within the stool might indicate bleeding higher in the digestive tract
- Blood that appears maroon or tarry black stools require immediate medical attention
When to Seek Medical Care
While some causes of blood in stool during constipation are relatively harmless, certain symptoms warrant prompt medical attention:
- Heavy bleeding or blood clots
- Severe abdominal or rectal pain
- Black, tarry stools
- Persistent bleeding lasting more than a few days
- Accompanying symptoms like fever or weight loss
- Age over 40 with new onset of bleeding
Treatment and Prevention Strategies
Several approaches can help manage constipation-related bleeding:
Lifestyle Modifications
Making dietary and lifestyle changes can significantly improve both constipation and related bleeding:
- Increasing fiber intake gradually
- Staying well-hydrated
- Regular physical activity
- Maintaining a consistent bathroom routine
Home Remedies
Several home treatments can help alleviate symptoms:
- Sitz baths for hemorrhoids and fissures
- Over-the-counter stool softeners
- Proper hygiene practices
- Gentle cleaning with unscented wipes
Frequently Asked Questions
What are common causes of blood in stool when I have constipation? The most common causes are hemorrhoids and anal fissures, which develop from straining during bowel movements and passing hard stools. These conditions typically cause bright red bleeding.
How can I tell if blood in my stool is from hemorrhoids or an anal fissure? Hemorrhoids usually cause painless bright red bleeding, while anal fissures typically cause sharp pain during bowel movements along with bleeding. The location and timing of pain can help distinguish between the two conditions.
When should I see a doctor if I notice blood in my stool while constipated? Seek immediate medical attention if you experience heavy bleeding, severe pain, black or tarry stools, persistent bleeding lasting more than a few days, or if you're over 40 with new onset of bleeding.
What are the best home treatments to stop bleeding from constipation-related anal fissures or hemorrhoids? Effective home treatments include sitz baths, increasing fiber intake, staying hydrated, using stool softeners, and maintaining good hygiene. Over-the-counter hemorrhoid creams may also help.
Can serious conditions like colorectal cancer cause constipation and blood in stool? Yes, while hemorrhoids and fissures are more common causes, serious conditions like colorectal cancer can cause both constipation and bleeding. This is why it's important to consult a healthcare provider, especially if you're over 40 or have additional concerning symptoms.