Brain stents have emerged as a crucial treatment option for managing brain aneurysms, offering hope to patients facing this serious neurological condition. Understanding the success rates, safety factors, and overall effectiveness of this innovative treatment is essential for both healthcare providers and patients considering this procedure.
This comprehensive guide explores the outcomes of brain stent procedures, examining success rates, safety considerations, and factors that influence treatment effectiveness. By understanding these aspects, patients and healthcare providers can make more informed decisions about their treatment options.
Understanding Brain Stent Success Rates
Clinical studies have shown encouraging success rates for brain stent procedures, particularly with pipeline embolization devices. Research indicates success rates ranging from 80% to 95% for unruptured aneurysms, with complete aneurysm occlusion often achieved within 6-12 months post-procedure.
Long-term follow-up studies demonstrate sustained effectiveness, with many patients experiencing permanent aneurysm closure and reduced risk of rupture. These positive outcomes have established brain stents as a preferred treatment option for certain types of brain aneurysms.
Safety Profile and Risk Assessment
The safety profile of brain stent procedures varies depending on several factors, including aneurysm location, size, and patient health status. For unruptured aneurysms, the procedure carries a relatively low risk profile, with major complications occurring in approximately 3-5% of cases.
Common Safety Considerations
- Procedure-related complications
- Medication response
- Recovery timeline
- Long-term monitoring requirements
Procedural Details and Implementation
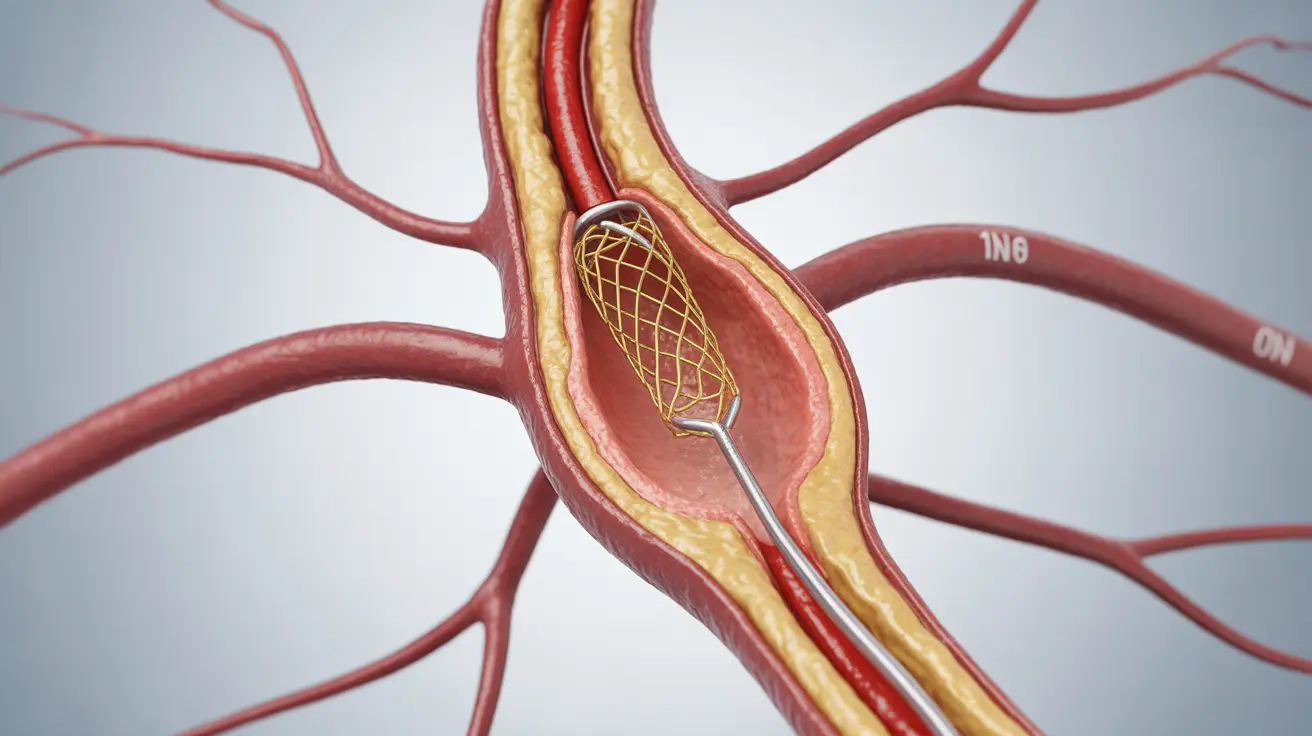
The brain stent placement procedure involves several careful steps performed by experienced neurovascular specialists. Using advanced imaging guidance, doctors navigate the stent through blood vessels to reach the affected area in the brain.
Key Procedural Steps
- Detailed pre-procedure imaging and planning
- Catheter-based stent delivery
- Precise positioning and deployment
- Immediate post-procedure monitoring
Factors Affecting Treatment Success
Several key factors can influence the success of brain stent procedures:
Patient-Related Factors
- Age and overall health status
- Aneurysm characteristics
- Medical history
- Medication compliance
Technical Factors
- Stent type and size selection
- Procedural expertise
- Facility capabilities
- Post-procedure care protocols
Recovery and Long-term Outcomes
Most patients experience positive long-term outcomes following brain stent procedures. Recovery typically involves a hospital stay of 2-4 days, followed by a gradual return to normal activities over several weeks.
Regular follow-up imaging and assessments help monitor the treatment's effectiveness and ensure optimal outcomes. Many patients report improved quality of life and reduced anxiety about aneurysm rupture risk.
Frequently Asked Questions
What is the success rate of pipeline stents in treating brain aneurysms?
Pipeline stents demonstrate success rates of 80-95% in treating brain aneurysms, with higher success rates observed in carefully selected cases. Complete aneurysm occlusion is typically achieved within 6-12 months post-procedure.
How safe is the pipeline stent procedure for unruptured and ruptured brain aneurysms?
The procedure is generally considered safe for unruptured aneurysms, with complication rates of 3-5%. For ruptured aneurysms, the risk profile is higher, and careful patient selection is crucial. The procedure's safety has improved significantly with advancing technology and surgical expertise.
What are the potential risks and complications associated with pipeline stents for brain aneurysms?
Potential complications include bleeding, stroke, device migration, and allergic reactions to medications. However, serious complications are relatively rare when procedures are performed by experienced practitioners in well-equipped facilities.
How is a pipeline stent placed in the brain, and what does the procedure involve?
The procedure involves accessing brain arteries through a small incision, typically in the groin area. Using advanced imaging guidance, specialists navigate the stent through blood vessels to the aneurysm location. The entire procedure usually takes 2-3 hours under general anesthesia.
What factors can affect the outcome or success of pipeline stent treatment for brain aneurysms?
Success factors include aneurysm size and location, patient age and health status, proper medication adherence, and the expertise of the treating team. Regular follow-up care and compliance with post-procedure instructions also significantly impact outcomes.