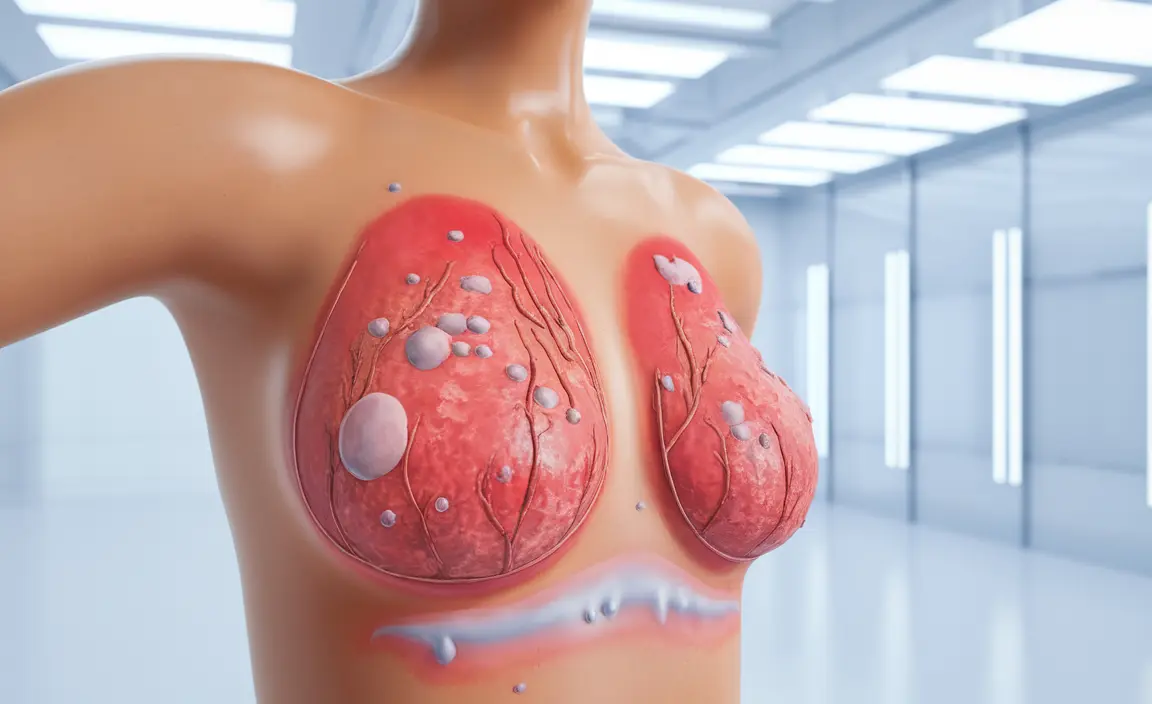
Breast eczema is a common skin condition that can cause significant discomfort and concern for those affected. This inflammatory skin condition can develop on and around the breasts, causing itching, redness, and various other symptoms that can impact daily life and emotional well-being.
Understanding the signs, causes, and treatment options for breast eczema is crucial for effective management and peace of mind. This comprehensive guide will help you identify symptoms, understand triggers, and explore various treatment approaches.
Understanding Breast Eczema Symptoms
Breast eczema presents with several distinctive symptoms that can help you identify the condition:
- Persistent itching and burning sensation
- Dry, scaly, or flaky skin patches
- Redness and inflammation
- Rough or leathery skin texture
- Small fluid-filled blisters that may weep
- Darkened or discolored skin areas
- Cracking or bleeding in severe cases
These symptoms may appear on any part of the breast, including the underside, between the breasts, or around the nipple area. The intensity can vary from mild to severe, and symptoms may come and go in episodes or flare-ups.
Common Causes and Triggers
Several factors can contribute to the development or worsening of breast eczema:
Environmental Triggers
- Extreme temperatures
- Low humidity
- Harsh soaps and detergents
- Synthetic fabrics
- Sweating during exercise
Medical Factors
- Allergies
- Hormonal changes
- Existing skin conditions
- Compromised immune system
- Family history of eczema
Treatment Approaches and Management
Managing breast eczema typically involves a combination of medical treatments and lifestyle modifications:
Medical Treatments
- Topical corticosteroids
- Moisturizing treatments
- Antihistamines for itching
- Prescription medications for severe cases
- Immunosuppressants when necessary
Self-Care and Prevention
Implementing proper self-care measures can help manage symptoms and prevent flare-ups:
- Use gentle, fragrance-free soaps
- Wear loose-fitting, breathable clothing
- Apply moisturizer immediately after bathing
- Keep the affected area clean and dry
- Avoid scratching or rubbing the affected skin
- Use hypoallergenic laundry products
Special Considerations for Breastfeeding
Breastfeeding mothers with breast eczema require particular attention to ensure both their comfort and their baby's safety:
- Choose baby-safe moisturizers and treatments
- Maintain good breast hygiene
- Consider using nursing pads made from natural materials
- Consult healthcare providers about safe treatment options
- Monitor for signs of infection
Frequently Asked Questions
What are the common symptoms of breast eczema and how can I recognize it? Breast eczema typically presents with itching, redness, dry or scaly patches, and possible inflammation. You may notice rough, leathery skin texture and small, fluid-filled blisters that can weep. The symptoms often appear in patches and may fluctuate in severity.
What causes breast eczema and which factors trigger flare-ups? Breast eczema can be triggered by various factors including allergies, hormonal changes, environmental conditions, stress, certain fabrics, soaps, and detergents. Sweat, heat, and friction can also contribute to flare-ups.
How is breast eczema treated and what home remedies can help manage it? Treatment typically involves a combination of topical medications, proper moisturizing, and trigger avoidance. Home remedies include using gentle, fragrance-free products, wearing breathable fabrics, and maintaining good skin hygiene. Cold compresses can help relieve itching and discomfort.
How can I tell the difference between breast eczema and breast cancer-related skin changes? While breast eczema typically causes itching, redness, and scaling that may come and go, breast cancer-related skin changes are usually persistent and may include dimpling, persistent redness, or nipple changes. Any concerning changes should be evaluated by a healthcare provider.
Can breastfeeding cause or worsen nipple eczema, and how can it be managed safely? Breastfeeding can potentially trigger or exacerbate nipple eczema due to moisture and friction. Safe management includes using appropriate moisturizers, maintaining good hygiene, using gentle nursing pads, and consulting with healthcare providers about safe treatment options while breastfeeding.