After a cesarean section (C-section), proper wound closure is crucial for healing and recovery. While both surgical staples and sutures are common methods for closing C-section incisions, each approach has distinct advantages and considerations that patients should understand.
This comprehensive guide explores the use of surgical staples in C-section procedures, including their benefits, potential risks, and proper wound care techniques to ensure optimal healing.
Understanding C-Section Staples
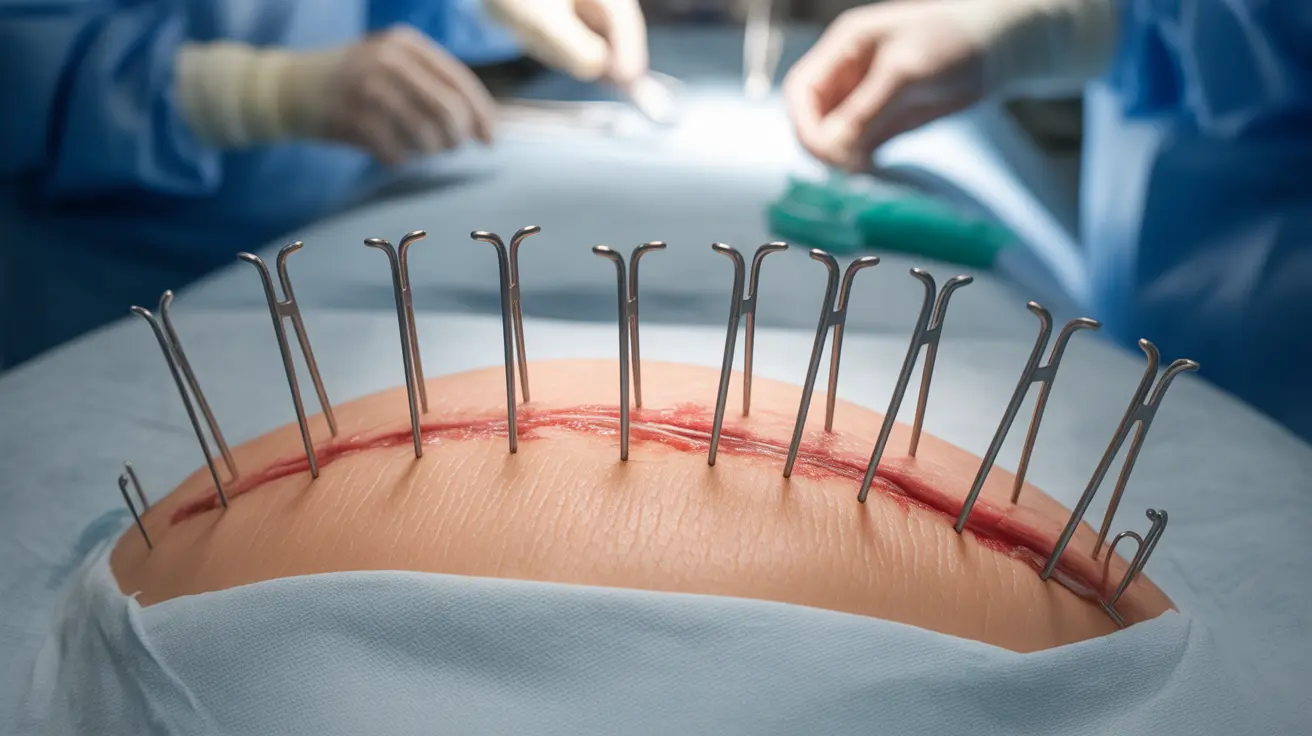
Surgical staples are medical devices made from sterile stainless steel or titanium that quickly and effectively close surgical incisions. During a C-section, doctors may choose staples for their speed of application and ability to secure multiple tissue layers simultaneously.
Advantages of Surgical Staples
C-section staples offer several benefits that make them an attractive option for surgical closure:
- Rapid application, reducing time in surgery
- Uniform wound closure
- Excellent tensile strength
- Reduced risk of needle stick injuries for medical staff
- Quick removal process
Comparing Staples to Sutures
The choice between staples and sutures often depends on various medical factors and surgeon preference. While staples can be applied more quickly, research suggests they may be associated with slightly different outcomes compared to traditional sutures.
Key Differences
Understanding the distinctions between these closure methods can help patients better prepare for their recovery:
- Healing time variations
- Cosmetic outcomes
- Pain levels during recovery
- Risk of complications
- Cost considerations
Staple Removal Process and Timeline
Typically, C-section staples remain in place for 3-5 days after surgery. The removal process is usually quick and straightforward, though some patients may experience mild discomfort.
What to Expect During Removal
The staple removal procedure involves:
- A healthcare provider using a special removal tool
- Quick extraction of each staple
- Application of Steri-strips or other wound closure strips
- Minimal discomfort lasting only moments
Post-Removal Wound Care
Proper wound care after staple removal is essential for preventing infection and promoting optimal healing. This includes keeping the incision site clean and dry, monitoring for signs of infection, and following all medical instructions carefully.
Frequently Asked Questions
What are the risks of using surgical staples for closing a C-section incision compared to sutures?
Surgical staples may carry a slightly higher risk of wound complications, including infection and wound separation. However, these risks can be minimized with proper wound care and monitoring. The main advantages include faster application time and consistent wound closure.
How long after a C-section are staples typically removed, and what should I expect during removal?
Staples are usually removed 3-5 days after surgery. The removal process takes about 5-10 minutes and involves using a specialized tool to gently remove each staple. While some patients may feel slight pressure or pinching, the procedure is generally well-tolerated.
Do surgical staples cause more pain or scarring than sutures after a C-section?
Pain levels can vary among individuals, but surgical staples typically don't cause significantly more pain than sutures. Regarding scarring, the final appearance often depends more on individual healing factors than the closure method used.
Why do doctors sometimes choose staples over sutures for C-section skin closure despite higher wound complication rates?
Doctors may opt for staples due to their quick application time, which reduces time under anesthesia and overall surgical duration. This can be particularly important in emergency situations or when dealing with certain risk factors that make shorter operating times preferable.
What are the best wound care practices to prevent infection after C-section staples are removed?
Key wound care practices include keeping the incision site clean and dry, changing dressings as directed, avoiding tight clothing over the wound, monitoring for signs of infection (redness, warmth, discharge, or increased pain), and following all post-operative care instructions provided by your healthcare team.