Low blood sugar, medically known as hypoglycemia, is commonly associated with diabetes treatment complications. However, many people don't realize that certain cancers can also trigger dangerous drops in blood glucose levels. While this connection is relatively uncommon compared to other causes of hypoglycemia, understanding when and how cancer can cause low blood sugar is crucial for early detection and proper treatment.
The relationship between cancer and hypoglycemia involves complex mechanisms that can significantly impact a person's health and quality of life. Recognizing the warning signs and understanding which types of cancer are most likely to cause these blood sugar drops can help patients and healthcare providers identify potential underlying malignancies more quickly.
How Cancer Can Lead to Hypoglycemia
Cancer can cause low blood sugar through several distinct mechanisms, each involving different ways that malignant tumors interfere with normal glucose regulation in the body. The most common pathway involves tumors that produce excessive amounts of insulin or insulin-like substances, which force blood sugar levels dangerously low.
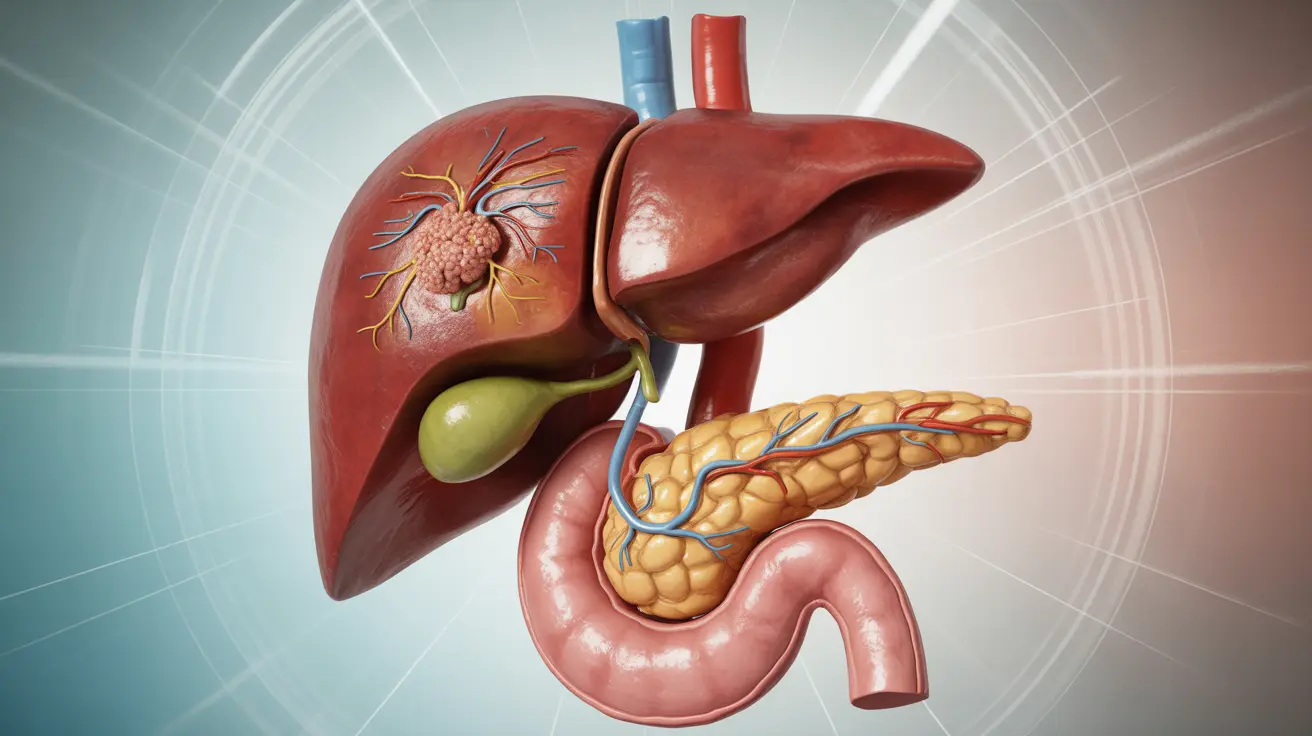
Some cancers consume large amounts of glucose for their rapid growth and metabolism. Large tumors, particularly those affecting the liver or other organs involved in glucose production, can essentially "steal" sugar from the bloodstream faster than the body can replenish it. This creates a situation where normal glucose reserves become depleted, leading to hypoglycemic episodes.
Additionally, certain tumors can interfere with the liver's ability to produce and release glucose when blood sugar levels drop naturally. Since the liver serves as the body's glucose repository and manufacturing center, any cancer that impairs liver function can disrupt the delicate balance needed to maintain stable blood sugar levels.
Types of Cancer Most Associated with Low Blood Sugar
Pancreatic Tumors
Pancreatic cancers, particularly insulinomas, represent the most well-known connection between malignancy and hypoglycemia. Insulinomas are tumors that develop in the insulin-producing cells of the pancreas and secrete excessive amounts of insulin into the bloodstream. While most insulinomas are actually benign, malignant versions can cause severe and persistent low blood sugar episodes.
Other pancreatic tumors, including pancreatic adenocarcinoma, can also affect blood sugar regulation, though they more commonly cause high blood sugar rather than hypoglycemia. The disruption occurs because these cancers can destroy the insulin-producing cells or interfere with normal pancreatic function.
Liver Cancer
Primary liver cancers and liver metastases from other cancers can significantly impact glucose homeostasis. The liver plays a central role in maintaining blood sugar levels by storing glucose as glycogen and releasing it when needed. Large liver tumors can impair these functions, leading to inadequate glucose production during periods when blood sugar naturally drops.
Large Abdominal Tumors
Massive tumors in the abdomen, regardless of their origin, can sometimes cause hypoglycemia through their sheer size and metabolic demands. These tumors may produce insulin-like growth factors or other substances that mimic insulin's effects, driving blood glucose levels down to dangerous ranges.
Blood Cancers
Certain blood cancers, including some types of lymphoma and leukemia, have been associated with hypoglycemia. These cancers can affect glucose metabolism through various mechanisms, including the production of antibodies that interfere with normal insulin function or through the massive consumption of glucose by rapidly dividing cancer cells.
Recognizing the Warning Signs
The symptoms of cancer-related hypoglycemia mirror those of low blood sugar from other causes, but they may be more persistent or severe. Early warning signs include excessive sweating, trembling or shaking hands, rapid heartbeat, and feelings of anxiety or irritability. These symptoms occur as the body attempts to compensate for falling blood glucose levels.
As hypoglycemia progresses, neurological symptoms become more prominent. Patients may experience confusion, difficulty concentrating, blurred vision, or coordination problems. Severe hypoglycemia can lead to loss of consciousness, seizures, or even coma if left untreated.
What distinguishes cancer-related hypoglycemia from other forms is often the pattern and persistence of symptoms. Unlike diabetic hypoglycemia, which typically responds well to glucose intake, cancer-related low blood sugar may be more difficult to correct and may recur frequently despite appropriate treatment.
When Low Blood Sugar Becomes a Red Flag
Several factors should prompt concern that hypoglycemia might be related to an underlying malignancy. Unexplained, recurrent episodes of low blood sugar in people without diabetes represent a significant warning sign that requires thorough medical evaluation.
The timing and severity of hypoglycemic episodes can also provide important clues. Cancer-related hypoglycemia often occurs during fasting periods or early morning hours when the body's glucose stores are naturally lower. Episodes that are difficult to treat with standard glucose interventions or that require frequent medical intervention should raise suspicion.
Additional concerning features include weight loss despite normal or increased appetite, persistent fatigue that doesn't improve with rest, or other systemic symptoms that accompany the hypoglycemic episodes. The presence of abdominal pain, changes in bowel habits, or jaundice alongside recurrent low blood sugar episodes particularly warrants cancer screening.
Diagnostic Approach and Treatment Considerations
When cancer is suspected as the cause of hypoglycemia, healthcare providers typically conduct comprehensive testing to identify potential malignancies. This may include advanced imaging studies such as CT scans or MRIs, blood tests to detect tumor markers, and specialized tests to measure insulin levels and related hormones.
Treatment of cancer-related hypoglycemia involves addressing both the immediate blood sugar management and the underlying malignancy. Short-term management focuses on preventing dangerous drops in blood glucose through dietary modifications, frequent monitoring, and sometimes medications that help maintain stable blood sugar levels.
Long-term treatment success depends largely on effectively treating the underlying cancer. For tumors like insulinomas, surgical removal often provides a cure and resolves the hypoglycemia completely. For other types of cancer, treatment may involve chemotherapy, radiation therapy, or other targeted interventions designed to shrink or eliminate the tumor causing the blood sugar disruption.
Frequently Asked Questions
Can cancer cause low blood sugar, and how common is this connection?
Yes, cancer can cause low blood sugar, though this connection is relatively uncommon. Cancer-related hypoglycemia occurs in less than 1% of all cancer cases, making it a rare but serious complication. The condition is most frequently associated with pancreatic tumors, particularly insulinomas, and large abdominal tumors that interfere with normal glucose metabolism.
What are the symptoms of low blood sugar caused by cancer?
Cancer-related low blood sugar produces symptoms similar to other forms of hypoglycemia, including sweating, trembling, rapid heartbeat, anxiety, confusion, blurred vision, and coordination difficulties. However, these symptoms may be more persistent, severe, or difficult to treat compared to typical diabetic hypoglycemia. Patients may also experience concurrent symptoms related to the underlying cancer, such as unexplained weight loss or persistent fatigue.
Which types of cancer are most likely to cause hypoglycemia?
Pancreatic cancers, especially insulinomas, are the most common cancer-related cause of low blood sugar. Liver cancers and large abdominal tumors also frequently cause hypoglycemia due to their impact on glucose metabolism and storage. Additionally, certain blood cancers like lymphoma and leukemia can occasionally lead to low blood sugar through various metabolic mechanisms.
How do pancreatic tumors like insulinomas cause low blood sugar?
Insulinomas cause low blood sugar by producing excessive amounts of insulin, the hormone responsible for lowering blood glucose levels. These tumors develop in the insulin-producing cells of the pancreas and secrete insulin continuously, regardless of blood sugar levels. This inappropriate insulin release forces glucose out of the bloodstream and into cells, creating dangerous drops in blood sugar that can occur even when fasting or between meals.
When should I be concerned that my low blood sugar might be a sign of cancer?
You should seek medical evaluation if you experience recurrent, unexplained episodes of low blood sugar, especially if you don't have diabetes or aren't taking medications known to cause hypoglycemia. Red flags include hypoglycemic episodes that are difficult to treat, occur frequently during fasting periods, or are accompanied by unexplained weight loss, persistent fatigue, or abdominal symptoms. Any pattern of low blood sugar that doesn't fit typical diabetic patterns warrants thorough medical investigation.