Dry eyes and inflammation are closely interconnected conditions that can create a challenging cycle of eye discomfort and irritation. When the eyes don't produce enough tears or when tears evaporate too quickly, it can trigger an inflammatory response that affects the eye's surface and surrounding tissues. Understanding this relationship is crucial for effective treatment and management of eye health.
This comprehensive guide explores the connection between dry eyes and inflammation, helping you recognize the symptoms and discover effective ways to manage this common condition. We'll examine both medical treatments and lifestyle changes that can provide relief and prevent long-term complications.
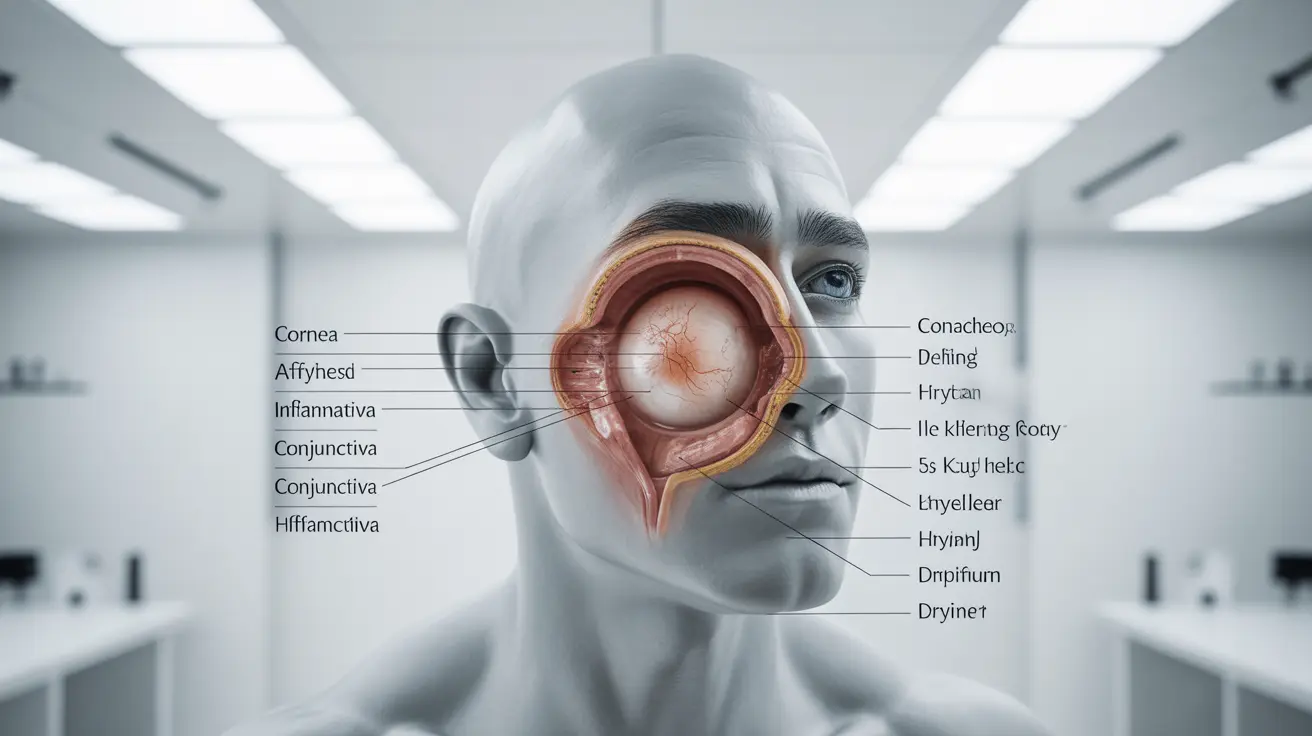
The Link Between Dry Eyes and Inflammation
When your eyes lack proper lubrication, the surface becomes irritated, triggering an inflammatory response. This creates a cycle where inflammation can further damage tear-producing glands, leading to even more dryness. The inflammation affects various parts of the eye, including the cornea, conjunctiva, and meibomian glands, which are essential for tear production and eye health.
Recognizing Symptoms of Dry Eye Inflammation
Identifying the signs of dry eye-related inflammation early can help prevent complications and ensure proper treatment. Common symptoms include:
- Redness and irritation
- Burning or stinging sensation
- Feeling of grittiness or foreign objects
- Light sensitivity
- Blurred vision
- Excessive tearing (as a reflex response)
- Eye fatigue
Treatment Options for Dry Eye Inflammation
Medical Interventions
Several medical treatments can effectively address both dryness and inflammation:
- Artificial tears and lubricating eye drops
- Anti-inflammatory medications
- Prescription eye drops (like Restasis or Xiidra)
- Steroid eye drops for severe cases
- Punctal plugs to retain tears
Natural and Supportive Treatments
Complementary approaches can enhance medical treatments and provide additional relief:
- Warm compresses for the eyes
- Gentle eyelid massage
- Omega-3 fatty acid supplements
- Proper eyelid hygiene
- Regular eye breaks during screen time
Environmental and Lifestyle Modifications
Making certain changes to your environment and daily habits can significantly reduce dry eye inflammation:
- Maintaining optimal humidity levels
- Using air filters to reduce irritants
- Taking regular breaks from digital devices
- Staying hydrated
- Protecting eyes from wind and sun
- Avoiding smoke and other irritants
Prevention and Long-term Management
Preventing dry eye inflammation requires a proactive approach to eye health:
- Regular eye examinations
- Consistent use of prescribed treatments
- Proper contact lens care and usage
- Balanced diet rich in eye-healthy nutrients
- Adequate sleep and stress management
Frequently Asked Questions
1. Can dry eyes cause inflammation and how does this affect the eye surface?
Yes, dry eyes can trigger inflammation of the eye surface. When tears are insufficient, the eye's surface becomes irritated, leading to inflammation that can damage the cornea and conjunctiva, potentially affecting vision and comfort.
2. What are the common symptoms that indicate dry eye-related inflammation?
Key symptoms include redness, burning sensation, feelings of grittiness, light sensitivity, blurred vision, and paradoxically, excessive tearing. These symptoms often worsen throughout the day.
3. How is inflammation from dry eye disease treated or managed effectively?
Treatment typically involves a combination of artificial tears, anti-inflammatory medications, prescription eye drops, and lifestyle modifications. Severe cases may require steroid drops or other medical interventions.
4. What lifestyle or environmental changes can help reduce dry eye inflammation?
Important changes include maintaining proper humidity levels, taking regular screen breaks, staying hydrated, protecting eyes from environmental irritants, and practicing good eye hygiene.
5. Can dry eye-related inflammation lead to long-term damage if left untreated?
Yes, untreated dry eye inflammation can lead to corneal damage, vision problems, and chronic eye discomfort. Early intervention and consistent management are essential to prevent long-term complications.