When blood sugar levels drop dangerously low, the brain and body can experience serious complications, including seizures. Understanding the connection between hypoglycemia and seizures is crucial, especially for individuals with diabetes or other conditions affecting blood sugar regulation.
This comprehensive guide explores how low blood sugar can trigger seizures, warning signs to watch for, and essential steps for prevention and treatment.
The Link Between Hypoglycemia and Seizures
Hypoglycemia occurs when blood glucose levels fall below 70 mg/dL. The brain relies heavily on glucose for proper functioning, and when levels drop severely (typically below 40 mg/dL), it can disrupt normal brain activity, potentially triggering seizures.
These seizures are the body's response to severe glucose deprivation in brain tissue, which can cause irregular electrical activity in the brain and lead to convulsions, loss of consciousness, and other neurological symptoms.
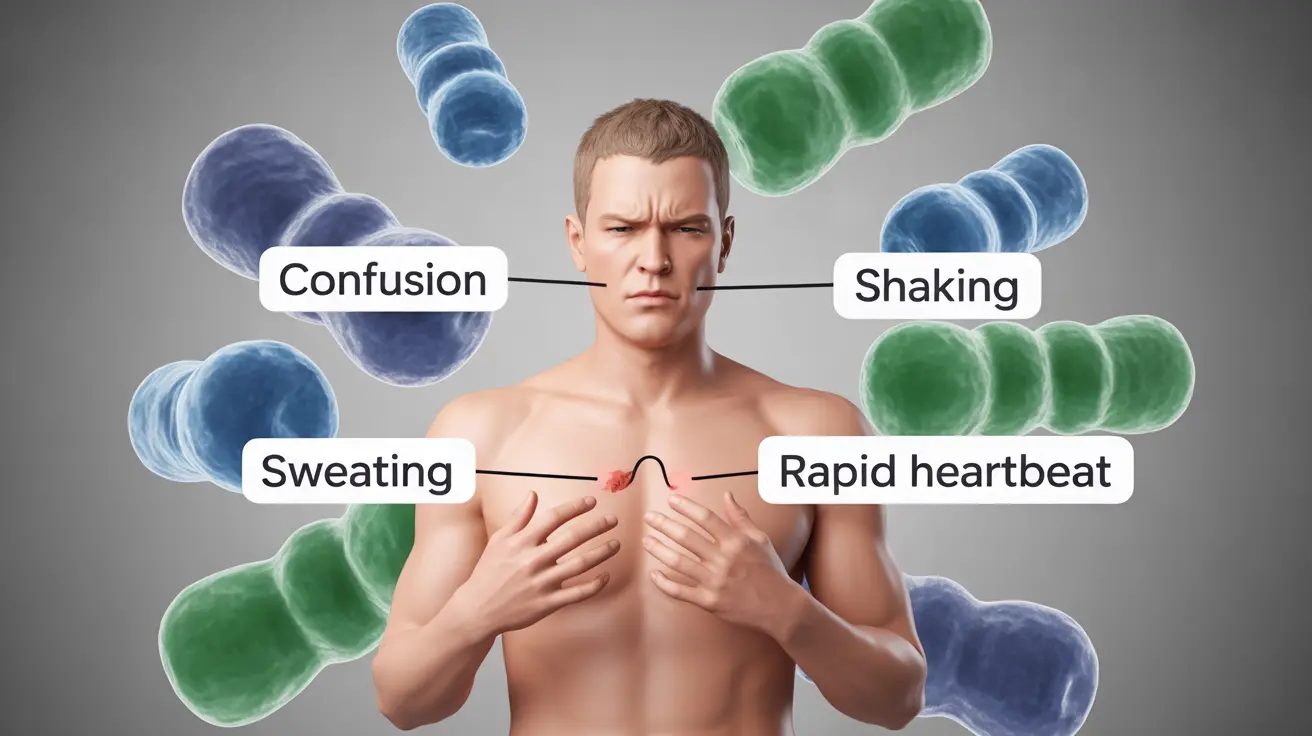
Warning Signs and Symptoms
Before a hypoglycemic seizure occurs, individuals often experience several warning signs:
- Confusion or difficulty concentrating
- Shakiness and trembling
- Excessive sweating
- Pale, clammy skin
- Rapid heartbeat
- Blurred or double vision
- Extreme hunger
- Anxiety or irritability
As blood sugar continues to drop, more severe symptoms may develop:
- Difficulty speaking or slurred speech
- Coordination problems
- Weakness or fatigue
- Changes in behavior or personality
- Loss of consciousness
High-Risk Groups
Certain individuals face a higher risk of experiencing hypoglycemic seizures:
- People with Type 1 diabetes
- Those taking insulin or certain diabetes medications
- Individuals with irregular eating patterns
- Athletes during intense physical activity
- Young children with diabetes
- People with reactive hypoglycemia
Treatment and Emergency Response
When someone experiences a hypoglycemic seizure, immediate action is crucial:
Immediate Steps
- Call emergency services (911)
- Place the person in the recovery position
- Do not put anything in their mouth
- Monitor breathing and consciousness
- Check blood sugar if possible
Post-Seizure Care
After the seizure ends, medical professionals will typically:
- Administer injectable glucagon
- Monitor blood glucose levels
- Provide intravenous glucose if necessary
- Evaluate for any injuries sustained during the seizure
Prevention Strategies
Preventing hypoglycemic seizures involves several key strategies:
- Regular blood sugar monitoring
- Consistent meal timing
- Proper medication management
- Carrying fast-acting glucose sources
- Wearing medical identification
- Education about early warning signs
Frequently Asked Questions
Can low blood sugar or hypoglycemia cause seizures?
Yes, severe hypoglycemia can cause seizures when blood glucose levels drop too low, typically below 40 mg/dL. This happens because the brain isn't receiving enough glucose to function properly.
What are the warning signs that hypoglycemia is leading to a seizure?
Warning signs include confusion, shakiness, sweating, pale skin, rapid heartbeat, blurred vision, and difficulty speaking. These symptoms often progress rapidly if blood sugar continues to drop.
How should I treat seizures caused by severe hypoglycemia?
Call emergency services immediately, place the person in the recovery position, and don't put anything in their mouth. Medical professionals will typically administer glucagon or intravenous glucose.
Who is most at risk of having seizures from low blood sugar?
People with Type 1 diabetes, those taking insulin or certain diabetes medications, individuals with irregular eating patterns, and young children with diabetes are at highest risk.
How can hypoglycemic seizures be prevented in people with diabetes?
Prevention involves regular blood sugar monitoring, consistent meal timing, proper medication management, carrying fast-acting glucose sources, and staying educated about warning signs.