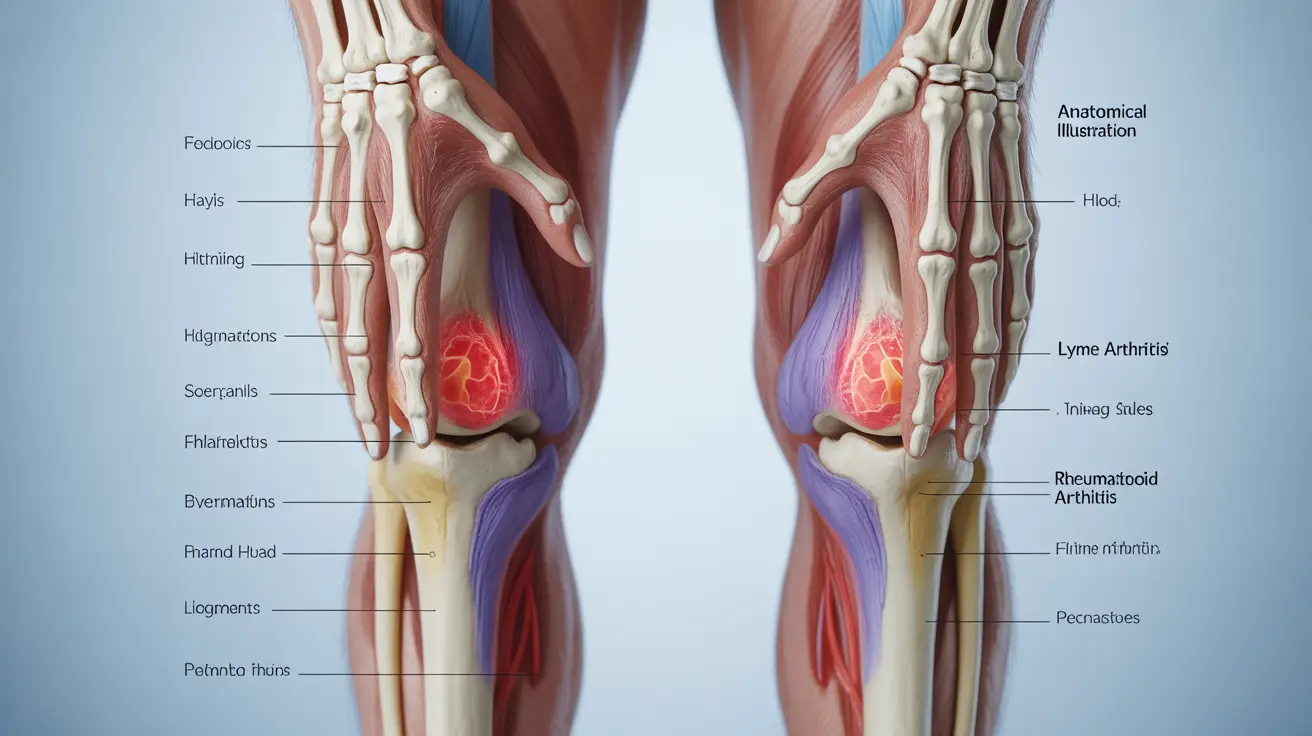
When dealing with joint pain and inflammation, understanding the relationship between Lyme disease and rheumatoid arthritis (RA) is crucial for proper diagnosis and treatment. While these conditions can present similar symptoms, they are distinct medical conditions that require different therapeutic approaches. This comprehensive guide explores their connection, differences, and treatment options.
The Link Between Lyme Disease and Joint Problems
Lyme disease, caused by the bacterium Borrelia burgdorferi and transmitted through tick bites, can affect multiple body systems, including the joints. When left untreated, approximately 60% of people with Lyme disease develop arthritis-like symptoms, particularly in large joints such as the knees.
Distinguishing Lyme Arthritis from Rheumatoid Arthritis
Symptom Patterns
Lyme arthritis typically presents with:
- Severe swelling in one or a few large joints
- Intermittent pain that may come and go
- Migration of symptoms from one joint to another
- Associated symptoms like fever, fatigue, and rash
Rheumatoid arthritis characteristically shows:
- Symmetrical joint involvement
- Persistent inflammation in multiple small joints
- Morning stiffness lasting over an hour
- Gradual onset of symptoms
Diagnostic Differences
Healthcare providers use different testing methods to distinguish between these conditions. Lyme disease diagnosis typically involves a two-tier blood testing approach to detect antibodies against B. burgdorferi. In contrast, RA diagnosis relies on physical examination, blood tests for rheumatoid factor and anti-CCP antibodies, and imaging studies.
Treatment Approaches
Treating Lyme-Related Joint Pain
The primary treatment for Lyme arthritis includes:
- Antibiotic therapy (typically doxycycline or amoxicillin)
- Anti-inflammatory medications
- Physical therapy when needed
- Regular monitoring of symptoms
Managing Rheumatoid Arthritis
RA treatment typically involves:
- Disease-modifying antirheumatic drugs (DMARDs)
- Biological response modifiers
- Long-term inflammation management
- Regular rheumatologist supervision
Prevention and Long-term Outlook
While RA cannot be prevented, Lyme disease prevention is possible through:
- Using insect repellent in tick-prone areas
- Wearing protective clothing
- Performing regular tick checks
- Removing ticks promptly if found
Frequently Asked Questions
Can Lyme disease cause rheumatoid arthritis or is it a separate condition?
Lyme disease and rheumatoid arthritis are separate conditions. While Lyme disease can cause joint inflammation (Lyme arthritis), it does not directly cause RA. However, some research suggests that Lyme infection might trigger autoimmune responses in susceptible individuals.What are the key differences between Lyme arthritis and rheumatoid arthritis symptoms?
Lyme arthritis typically affects one or a few large joints asymmetrically, often with episodic symptoms. Rheumatoid arthritis usually affects multiple small joints symmetrically with persistent inflammation and morning stiffness.How is Lyme arthritis diagnosed and distinguished from rheumatoid arthritis?
Diagnosis involves different blood tests: Lyme disease uses specific antibody tests for B. burgdorferi, while RA testing looks for rheumatoid factor and anti-CCP antibodies. Clinical presentation and history of tick exposure also play crucial roles in diagnosis.What treatments are effective for joint pain caused by Lyme disease compared to rheumatoid arthritis?
Lyme arthritis primarily requires antibiotic treatment, while RA needs long-term immunosuppressive therapy with DMARDs. Both conditions may benefit from anti-inflammatory medications, but their core treatments differ significantly.Can rheumatoid arthritis develop after having Lyme disease, and how common is this?
While some patients develop RA after Lyme disease, a direct causal relationship hasn't been definitively established. Studies suggest that Lyme infection might trigger autoimmune responses in genetically predisposed individuals, but this occurrence is relatively rare.