If you're experiencing persistent constipation, you might wonder about its underlying causes, including the possibility of colon polyps. While many factors can contribute to constipation, understanding the relationship between polyps and bowel habits is crucial for maintaining your digestive health.
In this comprehensive guide, we'll explore how colon polyps can affect your bowel movements, what symptoms to watch for, and when to seek medical attention. We'll also discuss diagnosis, treatment options, and important warning signs that shouldn't be ignored.
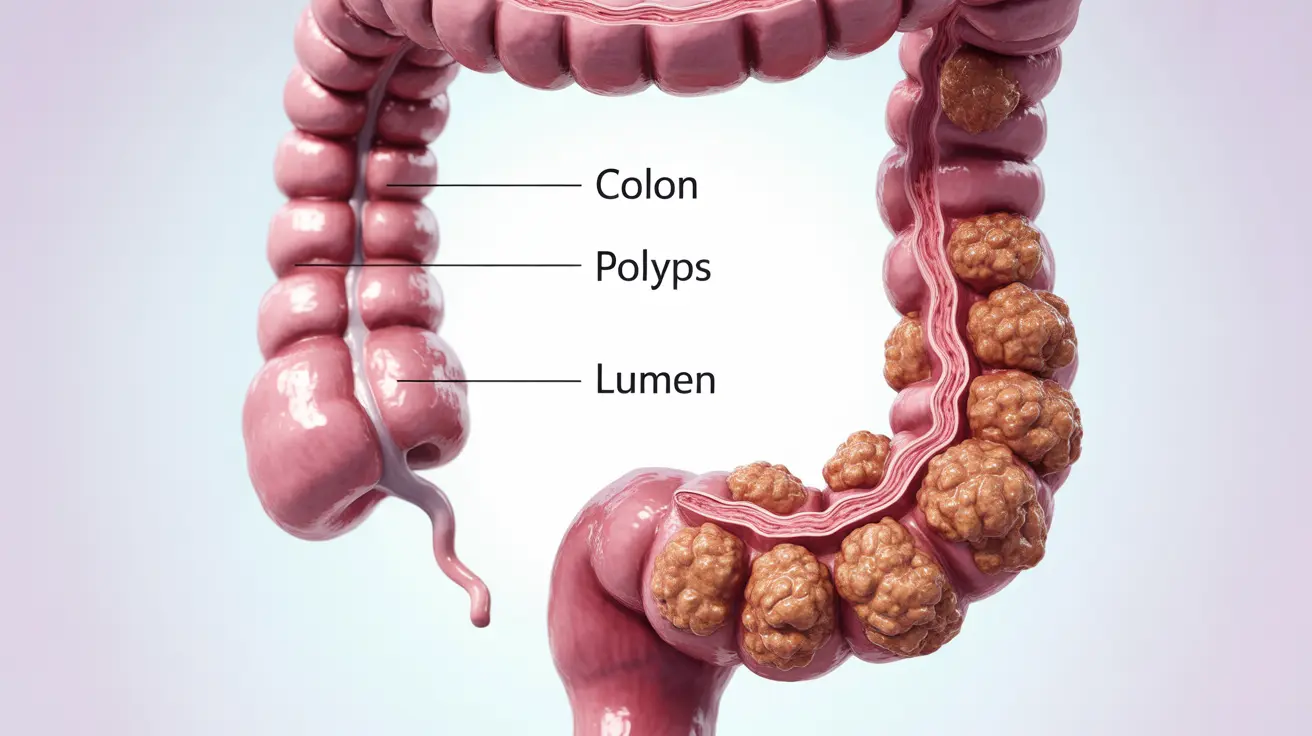
What Are Colon Polyps?
Colon polyps are small growths that develop on the inner lining of the large intestine (colon). These growths can vary in size from smaller than a pea to several inches in diameter. While most polyps are benign, some can develop into cancer over time, making early detection and monitoring essential.
How Polyps Affect Bowel Function
Large or numerous polyps can potentially interfere with normal bowel function in several ways:
- Physical obstruction of the intestinal passage
- Alteration of normal muscle contractions
- Changes in the colon's natural movement patterns
- Interference with normal water absorption
Common Symptoms Associated with Colon Polyps
While some people with colon polyps may experience no symptoms at all, others might notice various digestive changes, including:
- Changes in bowel habits
- Constipation or diarrhea
- Abdominal pain or cramping
- Blood in stool
- Unexplained weight loss
- Fatigue due to potential iron deficiency
Risk Factors and Prevention
Understanding your risk factors for developing colon polyps can help with prevention and early detection:
- Age (over 50)
- Family history of polyps or colorectal cancer
- Inflammatory bowel disease
- Unhealthy lifestyle habits (smoking, lack of exercise)
- Poor diet high in processed foods
Diagnosis and Treatment Options
Several diagnostic tools and procedures can help identify colon polyps:
Diagnostic Methods
- Colonoscopy
- Flexible sigmoidoscopy
- CT colonography
- Stool tests
Treatment Approaches
Treatment typically depends on the size, location, and number of polyps present. Common approaches include:
- Polypectomy during colonoscopy
- Minimally invasive surgery
- Regular monitoring and follow-up
- Lifestyle modifications
Frequently Asked Questions
Can large colorectal polyps cause constipation and changes in bowel habits?
Yes, large colorectal polyps can cause constipation and changes in bowel habits, particularly if they grow large enough to partially obstruct the colon. These changes might include difficulty passing stool, altered stool consistency, or irregular bowel movements.
What symptoms besides constipation should I watch for if I have colon polyps?
Key symptoms to watch for include rectal bleeding, changes in stool color or consistency, abdominal pain, unexplained weight loss, and fatigue. Any persistent change in bowel habits lasting more than a few weeks should be evaluated by a healthcare provider.
How are colorectal polyps that cause constipation diagnosed and treated?
Colorectal polyps are typically diagnosed through colonoscopy, which allows direct visualization of the colon. Other diagnostic tools may include CT scans or flexible sigmoidoscopy. Treatment usually involves removal of the polyps during colonoscopy or through surgery if they're particularly large.
Are larger polyps more likely to cause bowel obstruction or cancer?
Yes, larger polyps (typically over 1 cm) are more likely to cause bowel obstruction and have a higher risk of becoming cancerous. The size of a polyp is one of the key factors doctors consider when assessing risk and determining treatment approaches.
When should I see a doctor for constipation that might be related to polyps?
You should see a doctor if you experience persistent constipation lasting more than a few weeks, especially if it's accompanied by rectal bleeding, significant changes in bowel habits, unexplained weight loss, or severe abdominal pain. Anyone over 45 should also undergo routine colorectal cancer screening.