Portal hypertension is a serious medical condition that affects thousands of people worldwide, particularly those with liver disease. This condition occurs when blood pressure increases in the portal vein system, which carries blood from the digestive organs to the liver. Many patients and their families wonder whether this challenging condition can be reversed and what treatment options are available.
Understanding portal hypertension and its potential for reversal is crucial for making informed decisions about treatment and lifestyle modifications. While the answer isn't always straightforward, advances in medical treatment have provided new hope for managing this condition effectively and improving quality of life for those affected.
Understanding Portal Hypertension and Its Causes
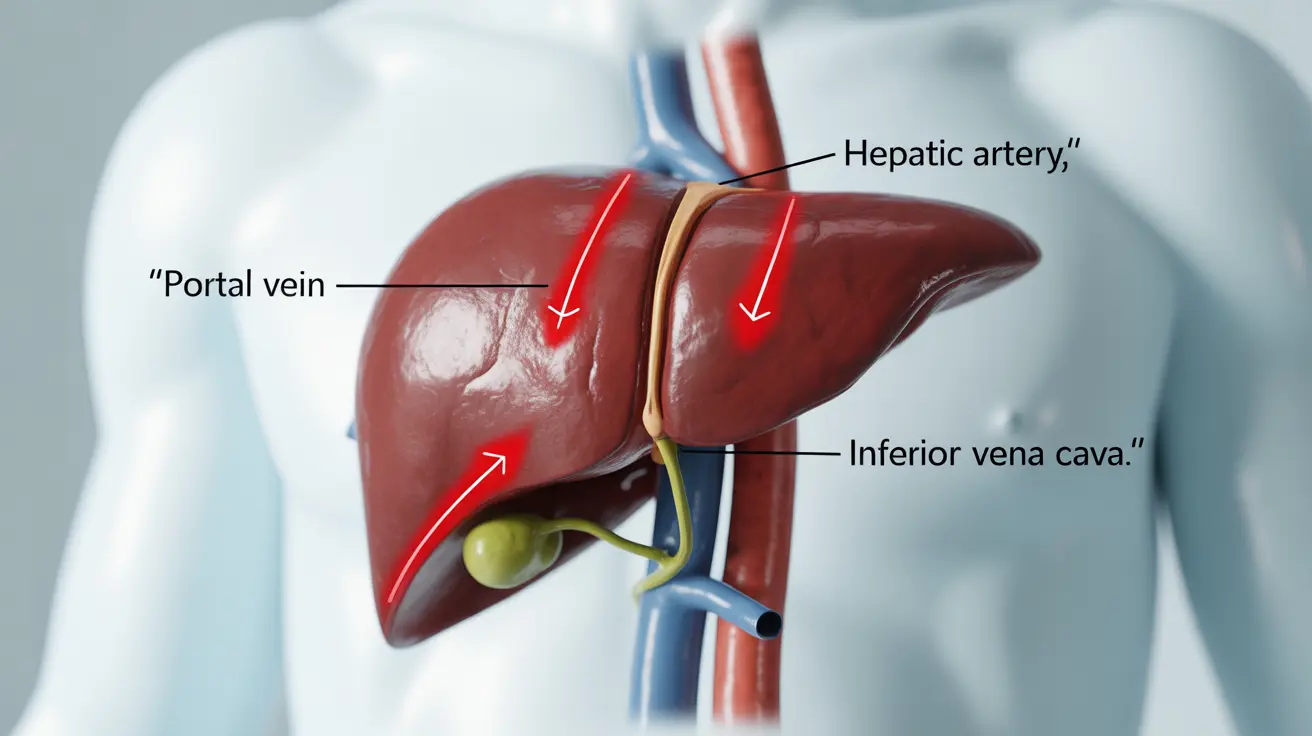
Portal hypertension develops when there is increased resistance to blood flow through the liver or blockages in the portal vein system. The most common cause is liver cirrhosis, which creates scar tissue that impedes normal blood flow. Other causes include blood clots in the portal vein, liver tumors, and certain infections.
The condition leads to serious complications including enlarged veins (varices) in the esophagus and stomach, fluid accumulation in the abdomen (ascites), and an enlarged spleen. These complications can be life-threatening if left untreated, making early intervention essential.
When liver tissue becomes scarred and hardened, it cannot function properly, and blood flow becomes restricted. This creates a backup of blood in the portal system, leading to increased pressure and the various symptoms associated with portal hypertension.
Can Portal Hypertension Be Reversed?
The reversibility of portal hypertension largely depends on its underlying cause and the extent of liver damage. In cases where the condition is caused by treatable factors such as blood clots, infections, or certain medications, addressing these root causes may lead to significant improvement or even reversal.
However, when portal hypertension results from liver cirrhosis, complete reversal is generally not possible because cirrhosis involves permanent scarring of liver tissue. The damaged liver tissue cannot regenerate to its original healthy state, meaning the structural changes that cause increased portal pressure remain.
Despite this limitation, early intervention and appropriate treatment can prevent further progression, reduce portal pressure, and significantly improve symptoms and quality of life. Some patients may experience partial improvement in portal pressure when the underlying liver disease is effectively managed.
Medical Treatments for Portal Hypertension
Several medical interventions can help manage portal hypertension and reduce complications. Beta-blockers, particularly propranolol and nadolol, are commonly prescribed medications that help lower portal vein pressure by reducing heart rate and cardiac output.
These medications work by blocking certain receptors in the cardiovascular system, leading to decreased blood flow to the portal circulation. Studies have shown that beta-blockers can reduce the risk of first-time variceal bleeding by approximately 40-50% when used consistently.
Diuretics may also be prescribed to help manage fluid retention and ascites, common complications of portal hypertension. These medications help the body eliminate excess fluid through increased urine production.
The TIPS Procedure
Transjugular Intrahepatic Portosystemic Shunt (TIPS) is a minimally invasive procedure that creates an artificial connection between the portal and hepatic veins within the liver. This shunt allows blood to bypass the scarred liver tissue, effectively reducing portal pressure.
TIPS is particularly effective for managing complications such as recurrent variceal bleeding and refractory ascites. The procedure involves inserting a small tube (stent) through a catheter, typically inserted through a vein in the neck, and positioning it to create the shunt within the liver.
Success rates for TIPS are generally high, with most patients experiencing significant reduction in portal pressure and improvement in symptoms. However, the procedure does carry risks, including the potential for hepatic encephalopathy, a condition where toxins normally filtered by the liver reach the brain.
Lifestyle Modifications and Prevention Strategies
While medical treatments are essential, lifestyle changes play a crucial role in managing portal hypertension and preventing its progression. The most important lifestyle modification is complete cessation of alcohol consumption, as alcohol can accelerate liver damage and worsen portal hypertension.
Maintaining a healthy diet low in sodium is vital for managing fluid retention and reducing the workload on the cardiovascular system. Patients should aim for less than 2 grams of sodium per day and work with healthcare providers to develop appropriate nutritional plans.
Regular monitoring and early treatment of hepatitis B and C can prevent the development of cirrhosis and subsequent portal hypertension. Vaccination against hepatitis A and B is recommended for those at risk.
Weight management is also important, as obesity can contribute to fatty liver disease, which may progress to cirrhosis. Engaging in appropriate physical activity, as recommended by healthcare providers, can help maintain overall health and liver function.
Prognosis and Long-term Management
The prognosis for portal hypertension varies significantly depending on the underlying cause, severity of liver damage, and response to treatment. Patients with early-stage disease who receive appropriate treatment often have better outcomes than those diagnosed in advanced stages.
Long-term management typically involves regular monitoring through blood tests, imaging studies, and endoscopic examinations to detect and treat complications early. Patients may need periodic adjustments to their medication regimens based on their response to treatment and disease progression.
For patients with end-stage liver disease, liver transplantation may be the most effective treatment option. Successful liver transplantation can essentially cure portal hypertension by replacing the diseased liver with a healthy one.
Frequently Asked Questions
Can portal hypertension caused by liver cirrhosis be reversed or cured?
Portal hypertension caused by liver cirrhosis cannot be completely reversed or cured because cirrhosis involves permanent scarring of liver tissue. However, treatments can significantly reduce portal pressure, manage complications, and improve quality of life. In cases of end-stage liver disease, liver transplantation offers the best chance for a cure.
What treatments are available to lower portal vein pressure and manage portal hypertension?
Several treatments can help lower portal vein pressure, including beta-blocker medications like propranolol and nadolol, which reduce cardiac output and portal blood flow. The TIPS procedure creates a shunt to bypass damaged liver tissue, while endoscopic treatments can address variceal bleeding. Diuretics help manage fluid retention, and liver transplantation may be considered for advanced cases.
How effective is the TIPS procedure in controlling complications of portal hypertension?
The TIPS procedure is highly effective in controlling complications of portal hypertension. It successfully reduces portal pressure in approximately 90% of patients and significantly decreases the risk of recurrent variceal bleeding. The procedure is also effective for managing refractory ascites, with most patients experiencing improvement in fluid retention within weeks of the procedure.
Are there medications that can reduce portal hypertension and prevent variceal bleeding?
Yes, beta-blockers such as propranolol and nadolol are the primary medications used to reduce portal hypertension and prevent variceal bleeding. These medications can reduce the risk of first-time bleeding by 40-50%. Additionally, proton pump inhibitors may be prescribed to reduce stomach acid production, and antibiotics might be used to prevent infections in high-risk patients.
What lifestyle changes or prevention strategies can help reduce the risk of developing portal hypertension?
Key prevention strategies include avoiding excessive alcohol consumption, maintaining a healthy weight, getting vaccinated against hepatitis A and B, practicing safe behaviors to prevent hepatitis transmission, and managing diabetes and other metabolic conditions. Early treatment of liver diseases, following a low-sodium diet, and regular medical monitoring can help prevent the progression of conditions that lead to portal hypertension.