The relationship between steroid medications and diabetes is a significant medical concern that affects many patients receiving corticosteroid treatment. While steroids are vital medications used to treat various conditions, from autoimmune disorders to inflammatory diseases, they can have profound effects on blood sugar regulation in the body.
Understanding how steroids might lead to diabetes, recognizing the risk factors, and knowing what to watch for can help patients and healthcare providers better manage this potential complication of steroid therapy.
How Steroids Affect Blood Sugar Levels
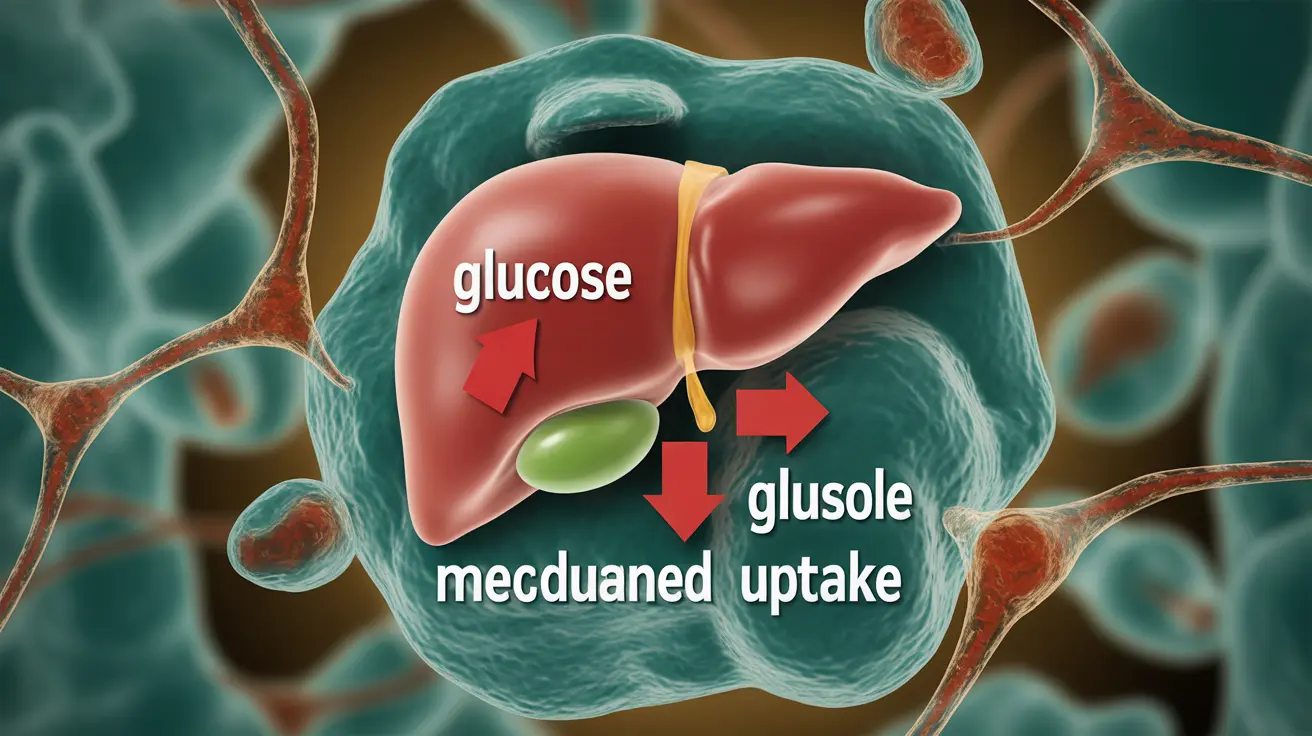
Corticosteroids work by mimicking the effects of naturally occurring hormones in your body. However, these medications can significantly impact how your body processes glucose, potentially leading to increased blood sugar levels through several mechanisms:
- Increased insulin resistance
- Enhanced glucose production in the liver
- Reduced glucose uptake in muscle tissue
- Interference with normal insulin secretion
Risk Factors for Steroid-Induced Diabetes
Certain individuals may be more susceptible to developing diabetes while taking steroid medications. Key risk factors include:
- Age (particularly those over 50)
- Family history of diabetes
- Obesity or overweight status
- High-dose steroid therapy
- Long-term steroid use
- Previous gestational diabetes
- Pre-existing impaired glucose tolerance
Recognizing the Warning Signs
Early detection of steroid-induced diabetes is crucial for proper management. Common symptoms that may indicate developing diabetes during steroid treatment include:
- Increased thirst and frequent urination
- Unexplained fatigue
- Blurred vision
- Slow wound healing
- Increased hunger
- Unexplained weight loss
Diagnosis and Monitoring
Healthcare providers typically monitor patients on steroid therapy through various methods:
- Regular blood glucose testing
- Glycated hemoglobin (A1C) measurements
- Fasting plasma glucose tests
- Random blood sugar checks
Management Strategies
Managing steroid-induced diabetes requires a comprehensive approach that may include:
- Blood sugar monitoring
- Dietary modifications
- Regular physical activity when appropriate
- Possible diabetes medications or insulin therapy
- Regular communication with healthcare providers
Prevention and Risk Reduction
While not all cases of steroid-induced diabetes can be prevented, certain strategies may help reduce the risk:
- Using the lowest effective steroid dose
- Taking steroids for the shortest necessary duration
- Maintaining a healthy weight
- Following a balanced diet
- Regular exercise (when medically appropriate)
Frequently Asked Questions
Can taking corticosteroids cause me to develop diabetes?
Yes, corticosteroid medications can cause diabetes by increasing insulin resistance and affecting how your body processes glucose. This condition is known as steroid-induced diabetes.
What are the common symptoms of steroid-induced diabetes to watch for?
Common symptoms include increased thirst, frequent urination, fatigue, blurred vision, slow wound healing, and unexplained weight changes. If you experience these symptoms while taking steroids, contact your healthcare provider.
How is steroid-induced diabetes diagnosed and managed?
Diagnosis involves blood glucose testing and A1C measurements. Management typically includes blood sugar monitoring, dietary changes, exercise when appropriate, and possibly diabetes medications or insulin therapy.
Are certain people more at risk of developing diabetes when using steroids?
Yes, risk factors include being over 50, having a family history of diabetes, obesity, receiving high-dose or long-term steroid therapy, and having pre-existing impaired glucose tolerance.
Can steroid-induced diabetes go away after stopping steroid treatment?
In many cases, blood sugar levels return to normal after discontinuing steroid therapy. However, some patients may develop persistent diabetes, particularly if they had pre-existing risk factors.
Remember to always discuss any concerns about steroid therapy and diabetes risk with your healthcare provider, who can help monitor your blood sugar and adjust treatment as needed.