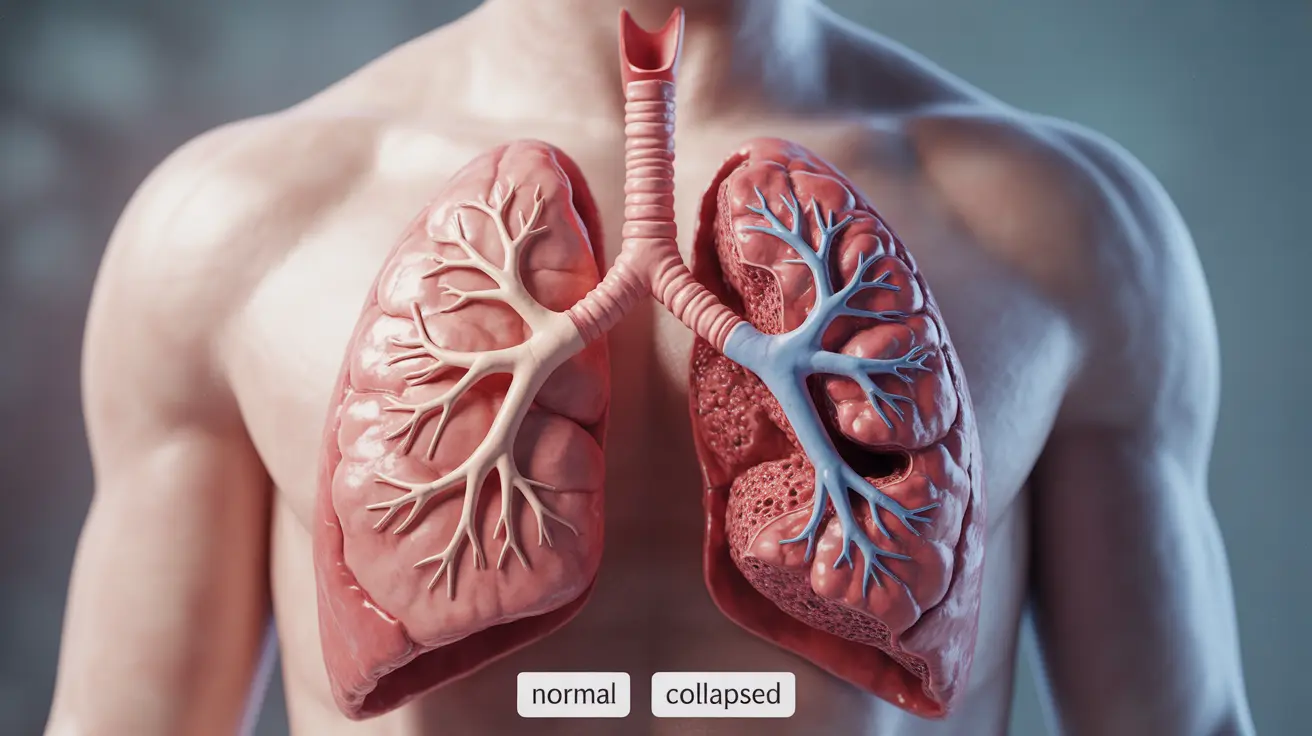
Atelectasis is a serious respiratory condition where parts of the lung collapse or become deflated, preventing normal oxygen exchange. This condition can affect anyone but is particularly common after surgery or in people with underlying lung conditions. Understanding what causes atelectasis in the lungs is crucial for both prevention and effective treatment.
What is Atelectasis and How Does It Develop?
Atelectasis occurs when the tiny air sacs (alveoli) in your lungs collapse or fill with fluid, preventing them from filling with air during breathing. This collapse can affect a small portion of the lung or, in more severe cases, an entire lobe, significantly impacting your ability to breathe effectively.
Common Causes of Atelectasis
Obstructive Atelectasis
This type occurs when something blocks the airway, preventing air from reaching the alveoli. Common obstructive causes include:
- Mucus plugs
- Foreign objects
- Tumors
- Enlarged lymph nodes
Non-obstructive Atelectasis
This form develops without a blockage and can result from:
- Chest injuries
- Pleural effusion (fluid around the lungs)
- Pneumothorax (collapsed lung)
- Extended bed rest
- Shallow breathing
Post-surgical Atelectasis
Surgery, especially procedures involving general anesthesia, is a leading cause of atelectasis. The combination of shallow breathing, lying flat, and the effects of anesthesia can lead to lung collapse.
Recognizing the Signs and Symptoms
The severity of symptoms often correlates with the extent of lung collapse. Common indicators include:
- Shortness of breath
- Rapid, shallow breathing
- Chest pain
- Coughing
- Bluish skin or lips (in severe cases)
Diagnostic Approaches
Healthcare providers use several methods to diagnose atelectasis:
- Chest X-rays
- CT scans
- Bronchoscopy
- Physical examination
- Blood oxygen level measurements
Treatment Options and Management
Immediate Interventions
Treatment focuses on re-expanding the collapsed lung tissue and addressing the underlying cause. Common approaches include:
- Deep breathing exercises
- Incentive spirometry
- Chest physiotherapy
- Position changes
- Bronchoscopy for obstruction removal
Long-term Management
Preventing recurrence often involves:
- Regular physical activity
- Proper positioning during rest
- Smoking cessation
- Treatment of underlying conditions
Prevention Strategies
Several measures can help prevent atelectasis, especially in high-risk situations:
- Early mobilization after surgery
- Regular deep breathing exercises
- Proper positioning during bed rest
- Maintaining good lung health
- Managing chronic respiratory conditions
Frequently Asked Questions
- What are the common causes of atelectasis in the lungs, and how does it affect breathing?
Atelectasis commonly results from airway obstruction, chest injuries, surgery, and prolonged bed rest. It affects breathing by reducing the lung's ability to exchange oxygen and carbon dioxide, leading to decreased oxygen levels in the blood.
- How is atelectasis diagnosed, and what are the typical tests used to confirm the condition?
Diagnosis typically involves chest X-rays, CT scans, and physical examination. Doctors may also use bronchoscopy to visualize the airways and measure blood oxygen levels to assess severity.
- What are the symptoms of atelectasis, and how do they differ based on the severity of lung collapse?
Symptoms range from mild to severe and include shortness of breath, chest pain, and coughing. More severe cases may present with rapid breathing, decreased oxygen levels, and bluish skin coloration.
- What are the most effective treatments for atelectasis, and how do they address the underlying cause?
Treatment effectiveness depends on the cause but typically includes deep breathing exercises, chest physiotherapy, and position changes. Severe cases may require bronchoscopy or surgery to remove blockages.
- Can atelectasis be prevented, especially after surgery or in individuals with chronic lung conditions?
Prevention strategies include early mobilization after surgery, regular deep breathing exercises, proper positioning, and management of underlying conditions. For those with chronic conditions, maintaining good lung health through regular exercise and avoiding smoking is crucial.