Being diagnosed with cervical cancer during pregnancy can be an overwhelming experience, raising serious concerns about both maternal and fetal health. Understanding the relationship between cervical cancer and pregnancy outcomes, particularly the risk of miscarriage, is crucial for expectant mothers facing this challenging situation.
This comprehensive guide explores how cervical cancer and its treatments can impact pregnancy, discussing the various risks and management strategies available to protect both mother and baby.
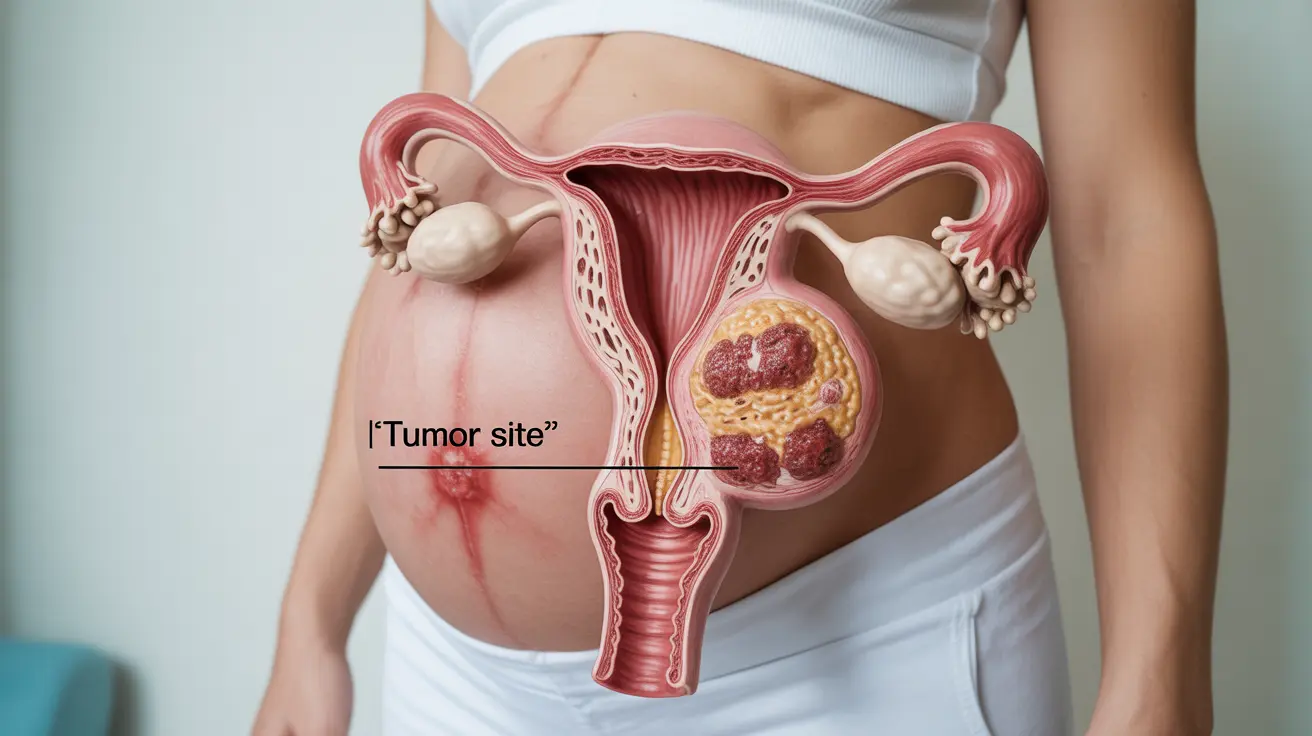
The Direct Impact of Cervical Cancer on Pregnancy
Cervical cancer itself rarely directly causes miscarriage in early pregnancy. However, as the cancer progresses, it can potentially affect pregnancy outcomes in several ways:
- Changes in cervical tissue structure
- Potential interference with placental development
- Increased risk of infection
- Possible complications during later stages of pregnancy
The location and stage of cervical cancer play significant roles in determining the level of risk to the pregnancy. Early-stage cancers generally pose less immediate threat to the developing fetus.
Treatment Considerations During Pregnancy
Timing of Treatment
The management of cervical cancer during pregnancy depends heavily on several factors:
- Stage of cancer
- Gestational age
- Patient's wishes regarding pregnancy continuation
- Overall health status
Healthcare providers must carefully balance the urgent need to treat cancer with protecting the pregnancy, often developing individualized treatment plans based on these factors.
Available Treatment Options
Treatment options vary depending on the cancer stage and pregnancy trimester:
- Careful monitoring (for very early-stage cancers)
- Surgery in select cases
- Modified chemotherapy protocols
- Delayed treatment until fetal viability
Managing Pregnancy Complications
Women with cervical cancer during pregnancy require specialized care to monitor and manage potential complications:
- Regular ultrasound monitoring
- Frequent cervical examinations
- Close monitoring of fetal development
- Specialized obstetric care
A multidisciplinary medical team typically coordinates care to ensure the best possible outcomes for both mother and baby.
Pregnancy Outcomes and Risk Factors
Several factors influence pregnancy outcomes when cervical cancer is present:
- Cancer stage at diagnosis
- Timing of diagnosis during pregnancy
- Type of treatment required
- Previous obstetric history
- Overall maternal health
Frequently Asked Questions
Can cervical cancer itself cause miscarriage during pregnancy?
While cervical cancer itself rarely directly causes early miscarriage, advanced cases may increase the risk of pregnancy complications. The primary concerns typically arise from necessary cancer treatments rather than the cancer itself.
How do treatments for cervical cancer affect the risk of miscarriage?
Certain cancer treatments can increase miscarriage risk, particularly in early pregnancy. Treatment choices are carefully tailored to minimize risks while effectively managing the cancer, often considering delayed treatment when possible.
Is chemotherapy safe during pregnancy if diagnosed with cervical cancer?
Certain chemotherapy protocols can be safely administered during pregnancy, particularly after the first trimester. However, treatment must be carefully selected and monitored to minimize risks to fetal development.
What pregnancy complications are associated with cervical cancer and its treatment?
Common complications include preterm labor, growth restriction, and delivery complications. The specific risks depend on cancer stage, treatment type, and timing of intervention.
How is cervical cancer managed during pregnancy to protect both mother and fetus?
Management involves a personalized approach with careful consideration of cancer stage, pregnancy timing, and individual circumstances. Treatment plans are developed by a multidisciplinary team to optimize outcomes for both mother and baby.
Understanding and managing cervical cancer during pregnancy requires careful coordination between oncology and obstetric care teams. Early detection and appropriate treatment planning are essential for optimizing outcomes for both mother and baby.