Cholesterol is one of the most discussed substances in health and medicine, yet many people remain unclear about its basic chemical identity. Understanding whether cholesterol is a carbohydrate, lipid, or protein forms the foundation for grasping its role in human health and disease prevention.
This classification isn't just academic—it directly impacts how cholesterol behaves in your body, how it's processed, and why it can both benefit and harm your cardiovascular system. Let's explore the science behind cholesterol's molecular structure and its far-reaching effects on your health.
The Chemical Identity of Cholesterol
Cholesterol is definitively classified as a lipid, specifically a type of sterol. This waxy, fat-like substance belongs to the lipid family due to its molecular structure, which consists primarily of carbon and hydrogen atoms arranged in a complex ring system. Unlike carbohydrates, which contain oxygen in a specific ratio to carbon and hydrogen, or proteins, which are built from amino acids, cholesterol's sterol structure places it firmly in the lipid category.
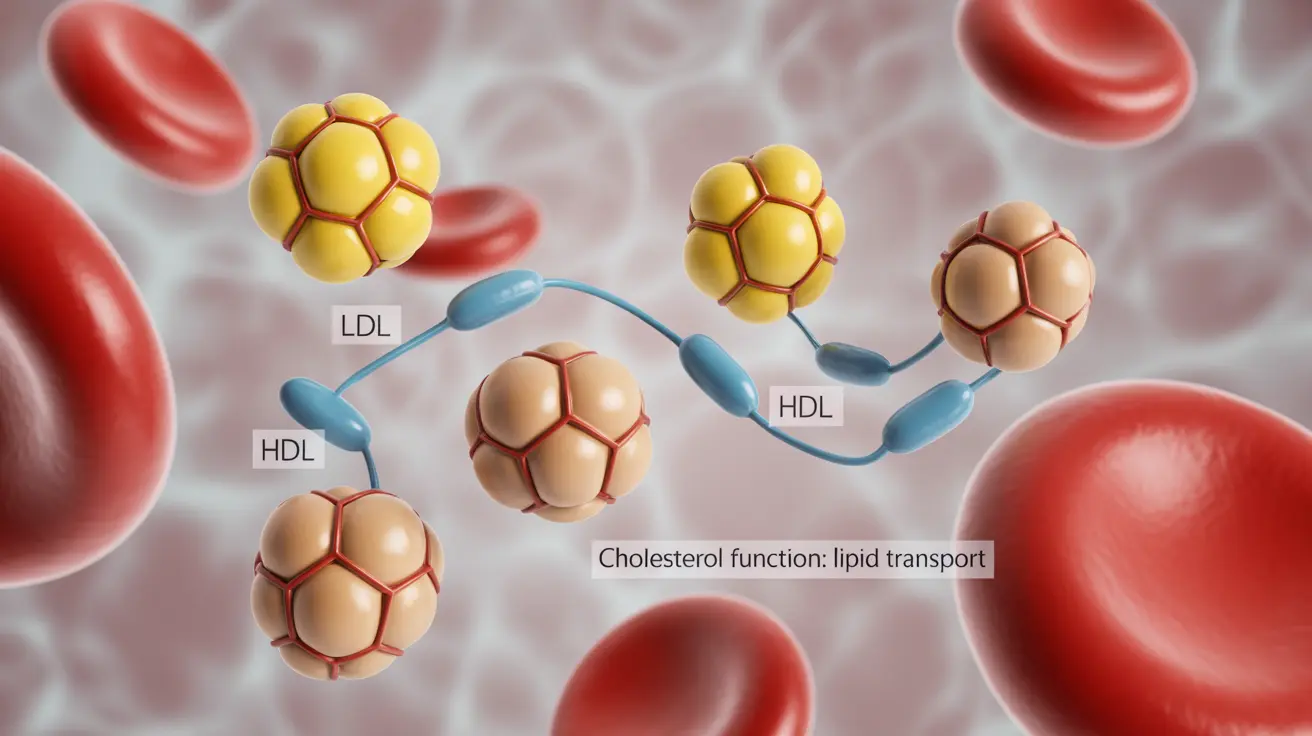
The classification matters because lipids have unique properties that affect how they move through your bloodstream and interact with cell membranes. Since cholesterol is not water-soluble like carbohydrates or many proteins, it requires special transport mechanisms—lipoproteins—to travel through your blood.
Essential Functions of Cholesterol in Your Body
Despite its negative reputation, cholesterol serves several critical functions that your body cannot perform without it. Your liver produces approximately 80% of the cholesterol your body needs, demonstrating just how essential this molecule is for normal physiological processes.
Cholesterol acts as a structural component of cell membranes, helping maintain their flexibility and integrity. It also serves as the precursor for several vital hormones, including testosterone, estrogen, and cortisol. Additionally, cholesterol is necessary for producing bile acids, which help digest dietary fats, and it plays a role in vitamin D synthesis.
These functions explain why your body maintains careful control over cholesterol production and why completely eliminating cholesterol isn't possible or desirable for optimal health.
Understanding LDL and HDL: The Good and Bad Cholesterol
The terms "good" and "bad" cholesterol actually refer to different types of lipoproteins that transport cholesterol through your bloodstream. Low-density lipoprotein (LDL) carries cholesterol from your liver to tissues throughout your body, while high-density lipoprotein (HDL) transports cholesterol back to your liver for processing or disposal.
LDL earns its "bad" reputation because elevated levels can lead to cholesterol accumulation in artery walls, contributing to atherosclerosis. When LDL particles become oxidized or modified, they're more likely to penetrate arterial walls and trigger inflammatory responses that promote plaque formation.
HDL is considered "good" because it performs the opposite function—removing excess cholesterol from peripheral tissues and arterial walls, then transporting it to the liver. This reverse cholesterol transport helps prevent cholesterol buildup in arteries and may even help remove cholesterol from existing plaques.
How High Cholesterol Contributes to Heart Disease
The pathway from high cholesterol to heart disease involves a complex cascade of events within your arterial walls. When LDL cholesterol levels remain elevated, these particles can penetrate the inner lining of arteries, particularly in areas where blood flow creates turbulence or stress.
Once inside the arterial wall, LDL particles may become oxidized by free radicals, making them more inflammatory and attractive to immune cells called macrophages. These cells attempt to clean up the oxidized cholesterol but can become overloaded, transforming into foam cells that contribute to plaque formation.
Over time, these plaques can grow larger, narrowing arteries and reducing blood flow to vital organs. If a plaque ruptures, it can trigger blood clot formation, potentially leading to heart attack or stroke. This process, called atherosclerosis, develops gradually over years or decades, often without obvious symptoms until significant blockages occur.
Natural Strategies for Optimizing Cholesterol Levels
Managing cholesterol levels effectively requires a multifaceted approach that addresses both LDL reduction and HDL improvement. Dietary modifications form the cornerstone of natural cholesterol management, with emphasis on reducing saturated fat intake while increasing consumption of fiber-rich foods, omega-3 fatty acids, and plant sterols.
Regular physical activity provides dual benefits by helping lower LDL cholesterol and raising HDL levels. Aerobic exercises like brisk walking, swimming, or cycling for at least 150 minutes per week can produce meaningful improvements in cholesterol profiles. Resistance training also contributes to better lipid management.
Weight management plays a crucial role, as excess body weight, particularly abdominal fat, can negatively impact cholesterol metabolism. Even modest weight loss of 5-10% can produce significant improvements in cholesterol levels. Additionally, avoiding trans fats, limiting refined carbohydrates, and maintaining consistent meal timing can support healthy cholesterol balance.
Frequently Asked Questions
Is cholesterol a lipid, carbohydrate, or protein, and why does the classification matter?
Cholesterol is a lipid, specifically a sterol, characterized by its waxy, fat-like molecular structure. This classification matters because it determines how cholesterol behaves in your body—since it's not water-soluble like carbohydrates, it requires special lipoprotein carriers to move through your bloodstream. Understanding this helps explain why cholesterol metabolism differs from other nutrients and why it can accumulate in arterial walls.
What is the difference between LDL and HDL cholesterol, and why is one called bad and the other good?
LDL (low-density lipoprotein) transports cholesterol from your liver to body tissues and can deposit cholesterol in artery walls, earning its "bad" designation. HDL (high-density lipoprotein) performs reverse cholesterol transport, removing excess cholesterol from tissues and arterial walls back to the liver, making it "good" cholesterol. The key difference lies in their direction of cholesterol transport and their impact on arterial health.
What functions does cholesterol serve in the body, and why do we need it despite health risks?
Cholesterol serves essential functions including maintaining cell membrane structure, producing vital hormones like testosterone and estrogen, creating bile acids for fat digestion, and supporting vitamin D synthesis. Your liver produces about 80% of needed cholesterol because these functions are critical for survival. The health risks arise from imbalanced levels, not from cholesterol's presence itself.
How does high cholesterol lead to heart disease and what happens in the arteries?
High LDL cholesterol can penetrate artery walls, where it may become oxidized and trigger inflammatory responses. Immune cells attempt to clean up this oxidized cholesterol but can become overloaded, forming foam cells that contribute to plaque buildup. These plaques narrow arteries and can rupture, potentially causing blood clots that lead to heart attacks or strokes.
What are the best ways to lower LDL cholesterol and raise HDL cholesterol naturally?
Natural cholesterol management includes reducing saturated fat intake, increasing fiber consumption, engaging in regular aerobic exercise for at least 150 minutes weekly, maintaining healthy body weight, and avoiding trans fats. Foods rich in omega-3 fatty acids, plant sterols, and soluble fiber specifically help lower LDL, while regular physical activity and moderate alcohol consumption (if appropriate) can help raise HDL levels.