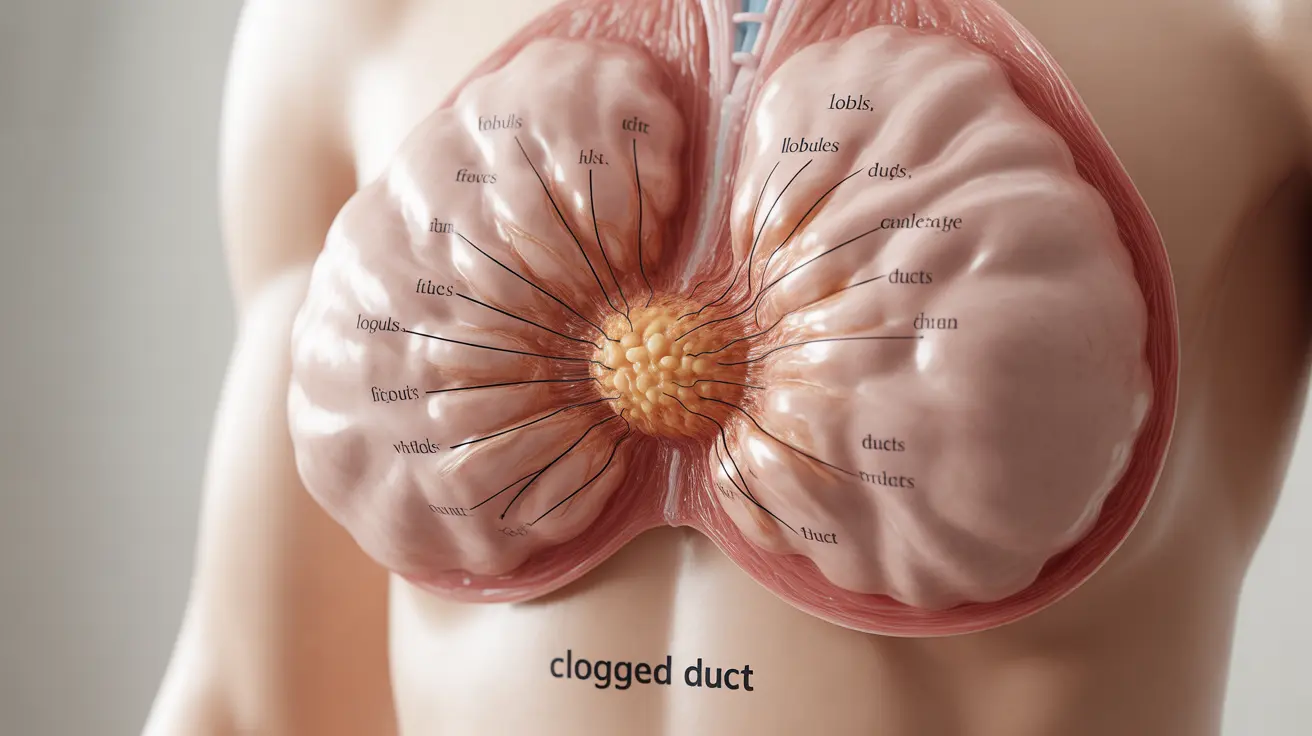
A clogged milk duct can be a painful and concerning experience for breastfeeding mothers. This common condition occurs when breast milk becomes trapped within a milk duct, causing discomfort and potentially interfering with successful breastfeeding. Understanding how to identify, treat, and prevent clogged milk ducts is essential for maintaining a healthy breastfeeding journey.
Understanding Clogged Milk Ducts
A clogged milk duct develops when breast milk becomes blocked within the milk ducts, typically appearing as a tender, firm lump in the breast tissue. This blockage can occur due to various factors, including inconsistent milk removal, tight clothing, or changes in feeding patterns. Early recognition and proper management are crucial to prevent more serious complications.
Common Signs and Symptoms
Recognizing the symptoms of a clogged milk duct early can help you take prompt action. Look for these characteristic signs:
- A tender or painful lump in the breast
- Localized redness in the affected area
- Warmth around the blocked duct
- Discomfort that may worsen during feeding
- Milk flow that appears slower from the affected breast
- Possible mild swelling in the affected area
Effective Home Treatment Methods
Most clogged milk ducts can be successfully treated at home with proper care and attention. Here are proven strategies to clear the blockage:
Frequent Nursing or Pumping
Continue breastfeeding or pumping regularly, starting with the affected breast. Position your baby so their chin points toward the clogged area, as this can help drain the duct more effectively.
Massage and Compression
Apply gentle massage to the affected area before and during feeding. Use a circular motion, working from the blocked area toward the nipple to help dislodge the clog.
Heat Application
Use warm compresses before feeding and take warm showers to help soften the blocked area. This can make it easier for the milk to flow and the blockage to clear.
Prevention Strategies
Taking proactive steps can help reduce your risk of developing clogged milk ducts:
- Ensure proper breast drainage during each feeding
- Wear comfortable, well-fitting bras without underwire
- Avoid sleeping on your stomach
- Stay well-hydrated and maintain a healthy diet
- Establish a consistent feeding schedule
- Address any latching issues promptly
When to Seek Medical Help
While most clogged ducts resolve with home treatment, certain symptoms warrant medical attention:
- Fever over 101.3°F (38.5°C)
- Severe pain or spreading redness
- Symptoms that persist beyond 48 hours
- Development of flu-like symptoms
- Pus or blood in breast milk
Frequently Asked Questions
What are the common symptoms of a clogged milk duct and how can I recognize it?
A clogged milk duct typically presents as a tender, firm lump in the breast, often accompanied by localized redness and warmth. You may notice discomfort during feeding and slower milk flow from the affected breast.
How can I treat a clogged milk duct at home to relieve pain and clear the blockage?
Effective home treatments include frequent nursing or pumping, gentle massage of the affected area, applying warm compresses, and ensuring proper breast drainage. Continue regular feeding sessions, starting with the affected breast.
What causes clogged milk ducts and how can I prevent them while breastfeeding?
Clogged ducts can be caused by inadequate milk removal, tight clothing, missed feedings, or poor latch. Prevention includes wearing comfortable bras, maintaining regular feeding schedules, ensuring proper latch, and staying well-hydrated.
When should I see a doctor for a clogged milk duct, and how can I tell if it has turned into mastitis?
Seek medical attention if you develop a fever, severe pain, spreading redness, or flu-like symptoms. These may indicate mastitis, a more serious infection requiring immediate treatment.
Can clogged milk ducts come back, and what steps can I take to manage recurring blockages?
Yes, clogged ducts can recur. Manage recurring blockages by identifying and addressing potential causes, maintaining good breastfeeding practices, and implementing preventive measures consistently. Consider working with a lactation consultant for personalized guidance.