Skin ulcers represent a significant health concern that affects millions of people worldwide, particularly those with underlying medical conditions or limited mobility. These open sores can develop for various reasons and understanding the different types is crucial for proper diagnosis and treatment.
This comprehensive guide explores the main categories of skin ulcers, their distinct characteristics, and the most effective treatment approaches for each type. Whether you're a healthcare provider, caregiver, or someone affected by skin ulcers, this information will help you better understand and manage these challenging conditions.
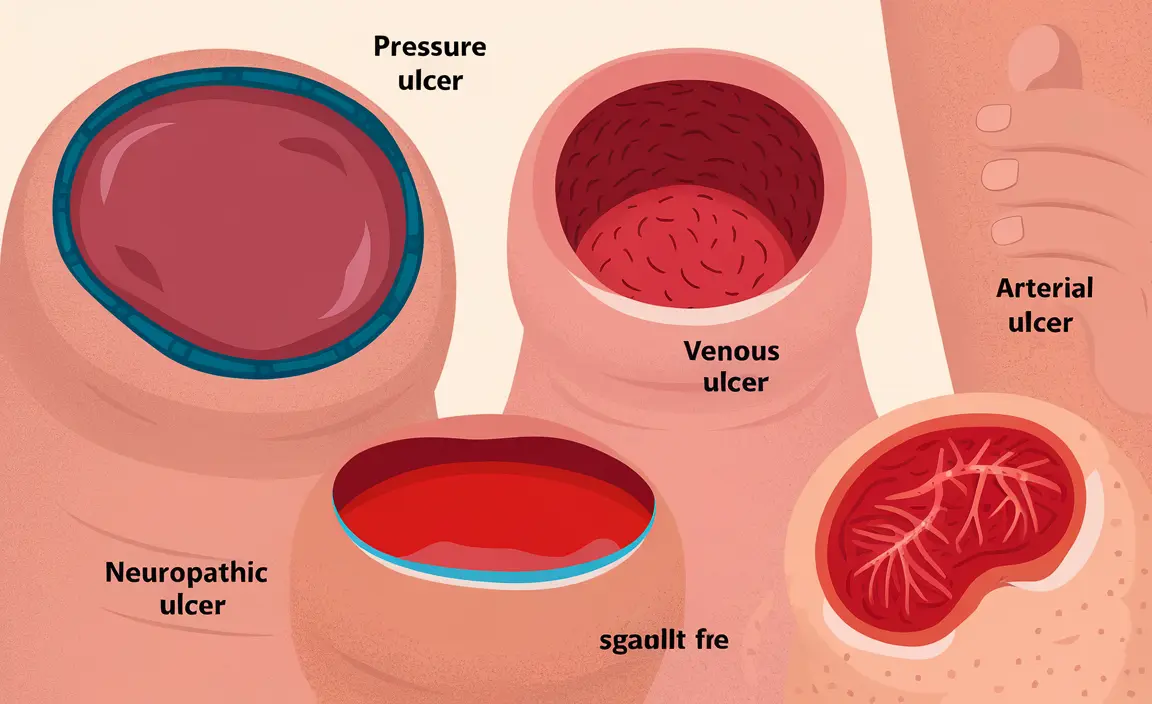
Types of Skin Ulcers and Their Characteristics
Understanding the distinct features of each type of skin ulcer is essential for proper identification and treatment. Here's a detailed look at the main categories:
Pressure (Decubitus) Ulcers
Pressure ulcers, also known as bedsores, typically develop in areas where bone creates pressure against the skin, especially when lying in one position for extended periods. Common locations include:
- Tailbone and sacrum
- Heels and ankles
- Hip bones
- Shoulder blades
These ulcers often appear as reddened areas initially, progressing to open wounds if left untreated.
Venous Ulcers
Venous ulcers occur due to poor circulation in the legs and are most commonly found in the lower leg area, particularly above the ankle. They typically present with:
- Shallow wound bed
- Irregular borders
- Surrounding skin discoloration
- Heavy drainage
- Associated leg swelling
Arterial Ulcers
Arterial ulcers develop due to insufficient blood flow to the tissues and are characterized by:
- Deep, punch-out appearance
- Well-defined borders
- Minimal drainage
- Pale wound bed
- Intense pain, especially when elevated
Neuropathic Ulcers
Most common in people with diabetes, neuropathic ulcers occur in areas of high pressure or trauma when sensation is decreased. They typically feature:
- Round or oval shape
- Thick callused border
- Located on pressure points of the feet
- Often painless due to nerve damage
Treatment Approaches and Management
Treatment strategies vary significantly depending on the type of ulcer and its underlying cause. Proper diagnosis is essential for effective treatment.
General Treatment Principles
All skin ulcers require certain basic care elements:
- Regular wound cleaning
- Appropriate dressing selection
- Infection prevention
- Pressure relief
- Management of underlying conditions
Specific Treatment Strategies
Each type of ulcer requires targeted interventions:
- Pressure ulcers: Regular repositioning and specialized support surfaces
- Venous ulcers: Compression therapy and leg elevation
- Arterial ulcers: Restoration of blood flow and careful wound care
- Neuropathic ulcers: Pressure relief and blood sugar control
Prevention Strategies
Preventing skin ulcers is crucial, especially for high-risk individuals. Key preventive measures include:
- Regular skin inspection
- Proper nutrition and hydration
- Pressure relief through repositioning
- Management of underlying health conditions
- Appropriate footwear and pressure relief devices
Frequently Asked Questions
What are the main differences between decubitus, venous, arterial, and neuropathic skin ulcers? The main differences lie in their causes and appearances. Decubitus ulcers result from pressure and appear over bony prominences. Venous ulcers occur due to poor circulation and appear on lower legs. Arterial ulcers result from poor blood flow and have a punched-out appearance. Neuropathic ulcers develop due to nerve damage and typically appear on pressure points of the feet.
How can I recognize the early signs and symptoms of the different types of skin ulcers? Early signs vary by type but generally include skin discoloration, tenderness, warmth, and changes in skin texture. Pressure ulcers begin as red areas that don't blanch, venous ulcers often show skin darkening and swelling, arterial ulcers may present with pain and cool skin, and neuropathic ulcers often develop under calluses.
What are the most effective treatments for pressure ulcers compared to venous or arterial ulcers? Pressure ulcers primarily require pressure relief and proper positioning, while venous ulcers respond best to compression therapy. Arterial ulcers need interventions to improve blood flow, often requiring surgical consultation. All types require appropriate wound care and dressing selection.
What causes neuropathic ulcers and why do they often occur in people with diabetes? Neuropathic ulcers occur due to nerve damage that reduces sensation, making individuals unaware of pressure or injury. In diabetes, high blood sugar levels can damage nerves over time, particularly in the feet, leading to reduced sensation and increased risk of unnoticed injuries that develop into ulcers.
How can skin ulcers be prevented, especially in older adults or people with limited mobility? Prevention strategies include regular repositioning every 2-4 hours, using pressure-relieving devices, maintaining good skin hygiene, ensuring proper nutrition, and managing underlying health conditions. Regular skin inspections and early intervention at the first sign of skin changes are crucial.