Head injuries and their potential complications are a significant concern in both sports medicine and general healthcare. One particularly concerning relationship is the connection between concussions and seizures. Understanding this link is crucial for anyone who has experienced a head injury or cares for those at risk of concussions.
In this comprehensive guide, we'll explore the relationship between concussions and seizures, including immediate and long-term risks, warning signs, and treatment options. This information is essential for patients, caregivers, and healthcare providers in managing post-concussion care effectively.
Understanding the Immediate Impact of Concussions
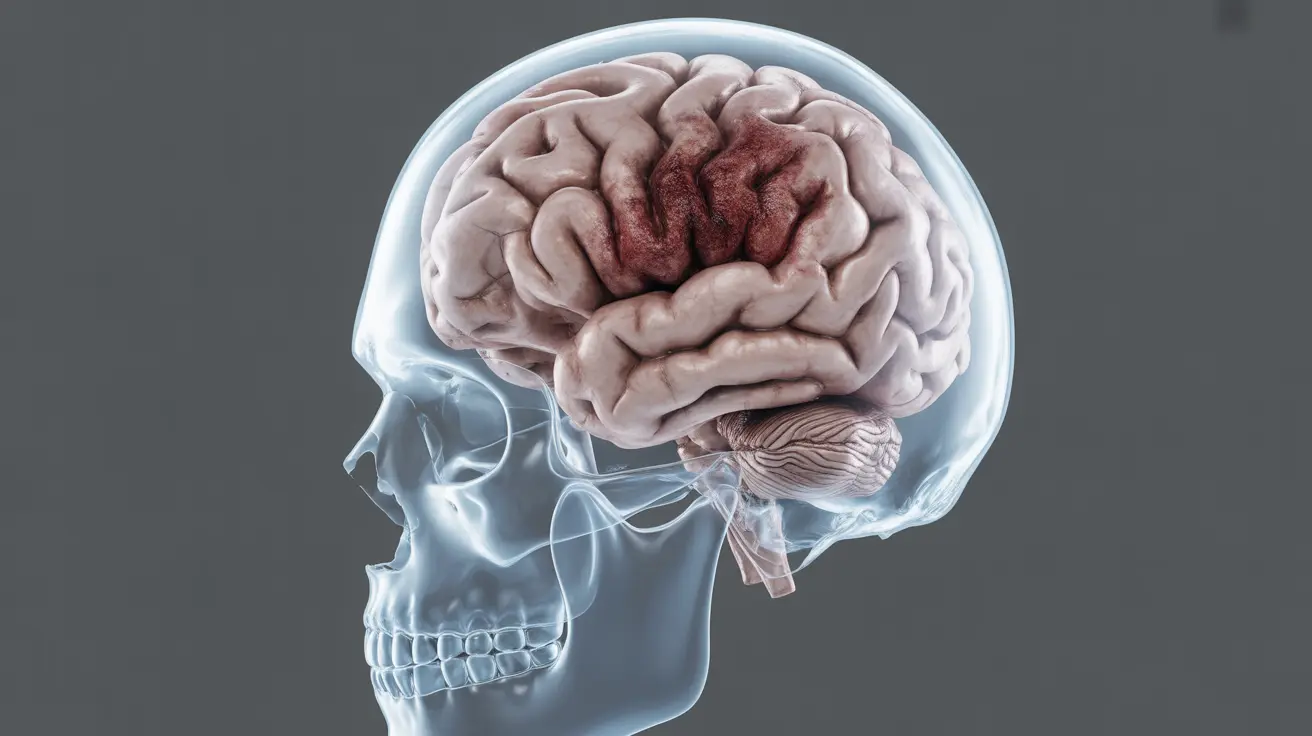
A concussion is a mild traumatic brain injury (mTBI) that occurs when the brain experiences sudden movement or impact within the skull. This trauma can temporarily disrupt normal brain function and potentially trigger various neurological symptoms, including seizures.
The immediate aftermath of a concussion can be particularly critical, as the brain is in a vulnerable state. During this period, the risk of experiencing a seizure may be elevated due to the disruption of normal electrical activity in the brain.
Types of Post-Concussion Seizures
Impact Seizures
These seizures occur immediately or within seconds of the head injury. They're generally considered less concerning for long-term complications but require immediate medical attention.
Early Post-Traumatic Seizures
Occurring within the first week after injury, these seizures indicate a more significant brain response to trauma and may require specific medical intervention and monitoring.
Late Post-Traumatic Seizures
These seizures develop after the first week following the injury and may indicate a higher risk of developing post-traumatic epilepsy.
Risk Factors for Post-Concussion Seizures
Several factors can increase the likelihood of experiencing seizures after a concussion:
- Severity of the head injury
- Location of the impact
- History of previous concussions
- Age at time of injury
- Presence of brain bleeding or contusion
- Genetic predisposition to seizures
Warning Signs and Symptoms
Being able to recognize potential seizure symptoms following a concussion is crucial. Key indicators include:
- Sudden confusion or disorientation
- Uncontrolled muscle spasms
- Loss of consciousness
- Unusual sensory experiences
- Memory gaps
- Temporary vision or hearing changes
Diagnosis and Medical Evaluation
Healthcare providers typically use several tools to assess seizure risk after a concussion:
- Detailed neurological examination
- EEG (electroencephalogram) monitoring
- Brain imaging (CT or MRI scans)
- Blood tests to rule out other conditions
- Careful review of the injury circumstances
Treatment Approaches
Treatment strategies for post-concussion seizures typically involve:
- Anti-epileptic medications when necessary
- Regular neurological monitoring
- Cognitive rest and gradual return to activities
- Lifestyle modifications to reduce seizure risk
- Prevention strategies for future head injuries
Frequently Asked Questions
- Can a concussion cause seizures immediately or only after some time?
Concussions can cause seizures both immediately after the injury and in the days, weeks, or months following the trauma. Immediate seizures (impact seizures) can occur at the moment of injury, while post-traumatic seizures may develop later.
- What are the risk factors that increase the chance of seizures after a concussion?
Key risk factors include the severity of the head injury, presence of brain bleeding, history of previous concussions, age, genetic predisposition to seizures, and the specific location of the head impact.
- How are seizures diagnosed and treated following a concussion?
Diagnosis involves neurological examinations, EEG monitoring, brain imaging, and careful symptom tracking. Treatment typically includes anti-epileptic medications, regular monitoring, and appropriate rest and recovery protocols.
- What symptoms should I watch for that might indicate a seizure after a head injury?
Important warning signs include sudden confusion, uncontrolled muscle movements, loss of consciousness, unusual sensory experiences, memory gaps, and changes in vision or hearing.
- Can a concussion lead to long-term epilepsy, and how common is this?
Yes, concussions can lead to long-term epilepsy, although this is relatively rare. The risk increases with the severity of the head injury and is more common in cases involving brain bleeding or significant trauma. Most people who experience a single, mild concussion do not develop long-term epilepsy.