Many people experience occasional constipation, but fewer realize that this common digestive issue can sometimes lead to unexpected symptoms, including lower back pain. The connection between bowel health and back discomfort is more significant than most people understand, involving complex anatomical relationships and pressure dynamics within the abdominal cavity.
Understanding how constipation can contribute to back pain empowers individuals to address both issues more effectively. This comprehensive guide explores the mechanisms behind constipation-related back pain, identifies key symptoms, and provides practical strategies for relief and prevention.
The Anatomical Connection Between Constipation and Back Pain
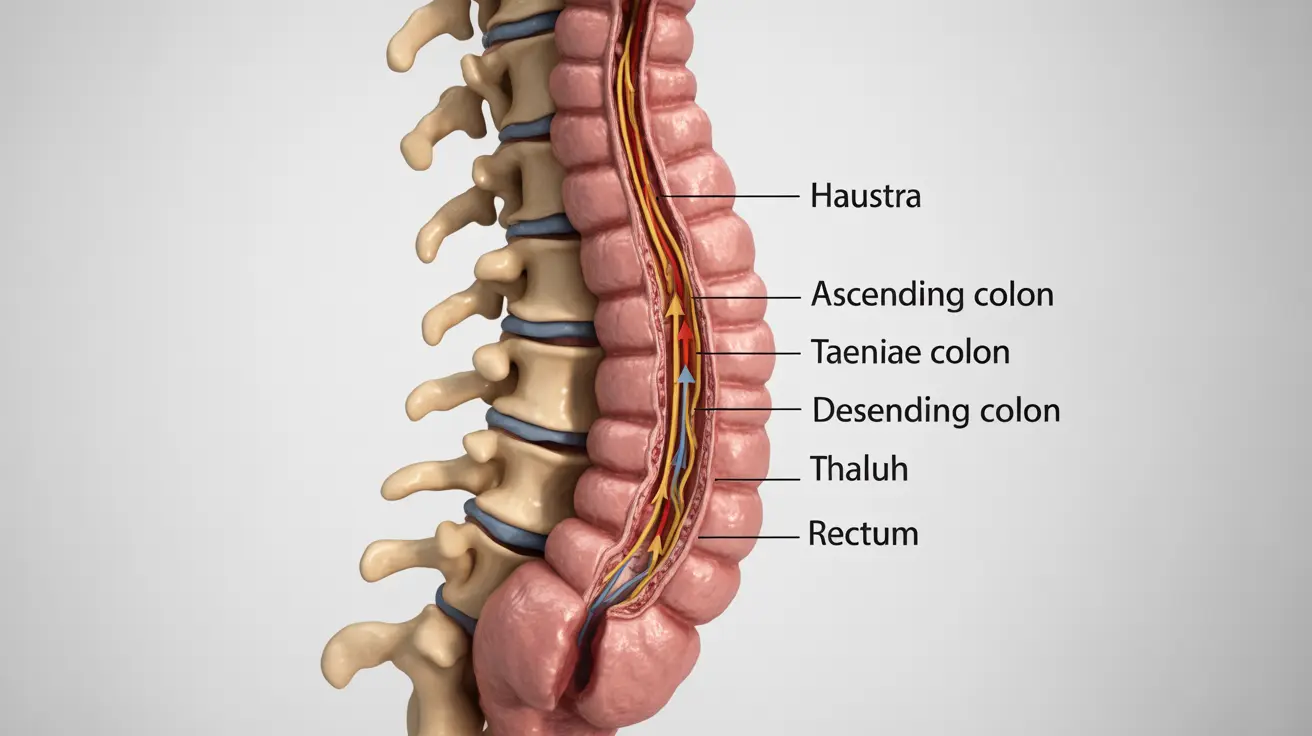
The relationship between constipation and back pain stems from the close anatomical proximity of the digestive system to the spine and surrounding muscles. When stool accumulates in the colon, it can create significant pressure within the abdominal cavity, affecting nearby structures including the lower back.
The colon sits directly in front of the lumbar spine, separated only by a thin layer of tissue. When constipation occurs, hardened stool can cause the colon to expand and press against the spine and surrounding nerves. This pressure can trigger pain signals that radiate to the lower back, creating discomfort that many people don't initially associate with their digestive issues.
Additionally, the muscles responsible for bowel movements are interconnected with core muscles that support the spine. When these muscles become strained from attempting to pass hard stool, the resulting tension can affect spinal alignment and contribute to back pain. The pelvic floor muscles, which play a crucial role in both bowel function and spinal stability, can become particularly affected during episodes of severe constipation.
How Constipation Triggers Lower Back Discomfort
Several mechanisms explain how constipation can lead to back pain. The primary cause involves increased intra-abdominal pressure, which occurs when stool builds up in the intestines. This pressure doesn't remain isolated to the digestive tract but affects the entire abdominal cavity, including structures that support the spine.
When the colon becomes distended with accumulated waste, it can compress nearby blood vessels and nerves. The lumbar plexus, a network of nerves that supplies the lower back and legs, can be particularly affected. This compression can result in referred pain, where discomfort is felt in areas distant from the actual source of the problem.
Straining during bowel movements also contributes to back pain through muscle tension and increased pressure on the spine. The Valsalva maneuver, which involves holding one's breath and bearing down, can significantly increase pressure within the abdominal cavity and place additional stress on the lower back structures.
Recognizing Constipation-Related Back Pain Symptoms
Identifying whether back pain stems from constipation requires understanding the distinct characteristics of this type of discomfort. Constipation-related back pain typically presents as a dull, aching sensation in the lower back that may worsen during periods of straining or when the bowel is particularly full.
The pain often coincides with other digestive symptoms, including bloating, abdominal distension, and the sensation of incomplete bowel evacuation. Unlike mechanical back pain from injury or poor posture, constipation-related discomfort may fluctuate with bowel movement patterns and dietary changes.
Key distinguishing features include:
- Pain that improves after successful bowel movements
- Discomfort that worsens with bloating or abdominal distension
- Associated digestive symptoms such as gas, cramping, or nausea
- Pain that may radiate to the sides or front of the abdomen
- Discomfort that responds to dietary modifications or increased fluid intake
Dietary and Lifestyle Solutions for Relief
Addressing constipation-related back pain requires a comprehensive approach focusing on improving bowel function while supporting overall digestive health. Dietary modifications form the foundation of effective treatment, with increased fiber intake being particularly beneficial.
Incorporating both soluble and insoluble fiber helps normalize stool consistency and promotes regular bowel movements. Excellent sources include fruits, vegetables, whole grains, and legumes. Gradually increasing fiber intake prevents digestive discomfort while allowing the digestive system to adapt to dietary changes.
Adequate hydration plays an equally important role in preventing and treating constipation. Water helps soften stool and supports the natural peristaltic movements of the intestines. Most adults benefit from consuming at least eight glasses of water daily, with additional fluids needed during hot weather or increased physical activity.
Regular physical activity stimulates bowel function through several mechanisms, including improved muscle tone, enhanced circulation, and optimized hormonal balance. Even gentle activities like walking, stretching, or yoga can significantly improve both digestive function and back pain symptoms.
Understanding Fecal Impaction and Severe Complications
Fecal impaction represents the most severe form of constipation, occurring when hardened stool becomes lodged in the colon and cannot be eliminated through normal bowel movements. This condition can cause intense back pain due to extreme pressure on surrounding structures and potential complications.
When fecal impaction occurs, the accumulated stool can form a large, hard mass that significantly distends the colon. This distension creates substantial pressure against the spine, potentially affecting nerve function and causing severe pain that may radiate throughout the lower back and into the legs.
Signs of fecal impaction include severe abdominal pain, inability to pass stool despite feeling the urge, nausea, vomiting, and intense back pain that doesn't improve with typical pain management strategies. This condition requires immediate medical attention, as it can lead to serious complications including bowel perforation or complete intestinal obstruction.
When to Seek Professional Medical Care
While mild constipation and associated back pain often respond well to home treatment, certain symptoms warrant immediate medical evaluation. Persistent constipation lasting more than a few days, particularly when accompanied by severe back pain, requires professional assessment to rule out underlying conditions.
Warning signs that indicate the need for urgent medical care include fever, severe abdominal pain, vomiting, blood in the stool, or sudden onset of severe back pain. These symptoms may indicate complications such as bowel obstruction, infection, or other serious conditions requiring immediate intervention.
Individuals with chronic constipation should also seek medical evaluation to identify potential underlying causes and develop an appropriate treatment plan. Conditions such as irritable bowel syndrome, thyroid disorders, or neurological conditions can contribute to chronic constipation and may require specialized treatment approaches.
Frequently Asked Questions
Can constipation cause lower back pain and why does this happen?
Yes, constipation can definitely cause lower back pain. This occurs because the colon sits directly in front of the lumbar spine, and when stool accumulates, it creates pressure that can press against the spine and surrounding nerves. The increased intra-abdominal pressure from constipation affects the entire abdominal cavity, including structures that support the spine, leading to referred pain in the lower back.
What are the symptoms that indicate constipation-related back pain versus other causes of back pain?
Constipation-related back pain typically presents as a dull ache that coincides with digestive symptoms like bloating and abdominal distension. Unlike mechanical back pain, this discomfort often improves after bowel movements and worsens with straining. It may also be accompanied by gas, cramping, and the sensation of incomplete evacuation, and tends to respond to dietary changes and increased fluid intake.
How can I relieve back pain caused by constipation through diet and lifestyle changes?
Relief can be achieved by increasing fiber intake through fruits, vegetables, and whole grains, while ensuring adequate hydration with at least eight glasses of water daily. Regular physical activity, even gentle walking or stretching, helps stimulate bowel function. Establishing regular bathroom habits and avoiding straining during bowel movements also helps reduce both constipation and associated back pain.
When should I see a doctor if my constipation and back pain do not improve or get worse?
Seek medical attention if constipation persists for more than a few days with severe back pain, or if you experience warning signs such as fever, severe abdominal pain, vomiting, blood in stool, or sudden onset of intense back pain. Chronic constipation lasting weeks or recurring frequently also warrants professional evaluation to identify underlying causes and develop appropriate treatment.
What is fecal impaction and how does it relate to severe back pain in constipation cases?
Fecal impaction occurs when hardened stool becomes lodged in the colon and cannot be eliminated naturally. This creates a large, hard mass that significantly distends the colon, causing extreme pressure against the spine and potentially affecting nerve function. The resulting back pain is typically severe and may radiate into the legs. This condition requires immediate medical attention due to risk of serious complications like bowel perforation.