Menopause brings numerous changes to a woman's body, and digestive issues like constipation are among the most common yet often overlooked symptoms. The connection between constipation and menopause affects millions of women worldwide, with studies showing that up to 60% of postmenopausal women experience some form of digestive discomfort.
Understanding why this happens and knowing effective management strategies can significantly improve quality of life during this natural transition. From hormonal fluctuations to lifestyle factors, multiple elements contribute to digestive changes during menopause, making it essential to address both the underlying causes and practical solutions.
How Hormonal Changes During Menopause Affect Digestion
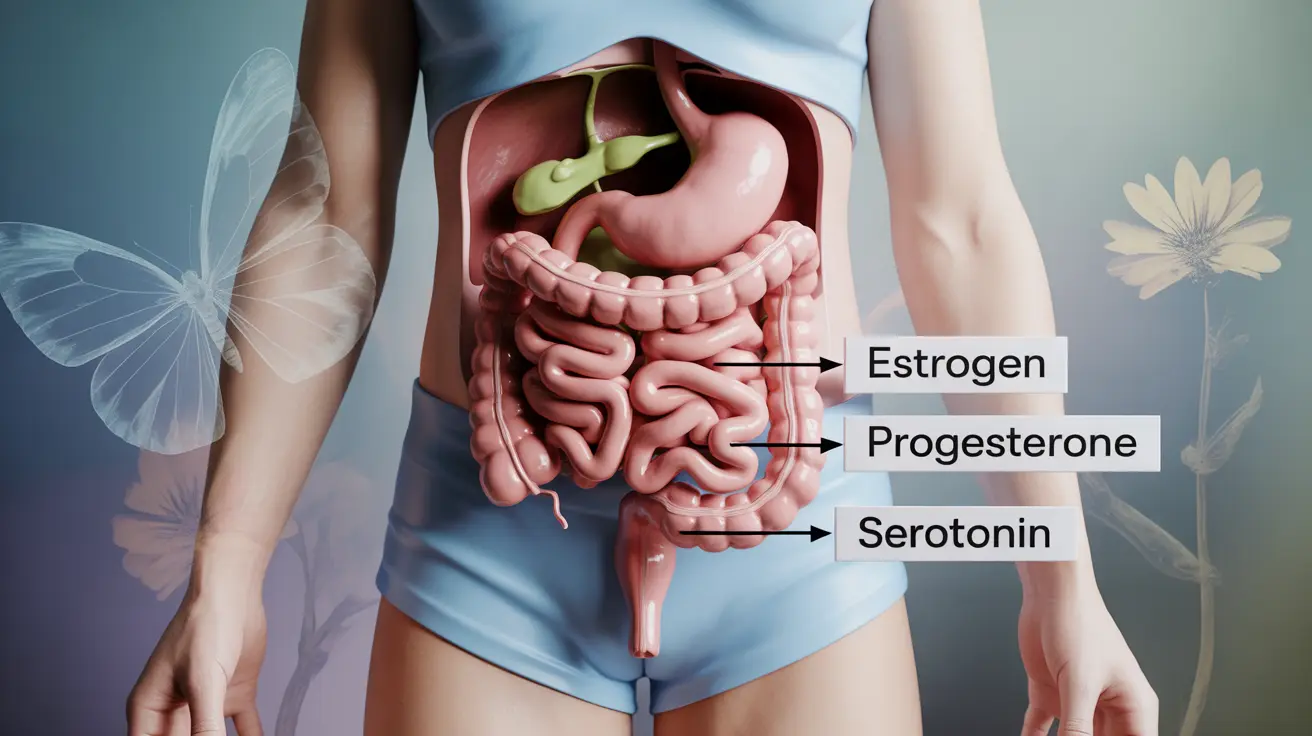
The relationship between constipation and menopause stems primarily from declining estrogen and progesterone levels. These hormones play crucial roles in maintaining healthy digestive function throughout a woman's reproductive years.
Estrogen helps regulate the production of digestive enzymes and maintains healthy gut motility. When levels drop during perimenopause and menopause, the digestive tract can slow down significantly. This reduction in motility means food moves more slowly through the intestines, allowing more water to be absorbed and resulting in harder, more difficult-to-pass stools.
Progesterone also influences digestive health by affecting smooth muscle contractions in the intestinal wall. Lower progesterone levels can lead to weaker muscle contractions, further contributing to slower transit times and increased constipation risk.
Additional Factors Contributing to Digestive Changes
Beyond hormonal fluctuations, several other menopause-related factors can worsen constipation. Decreased physical activity, often due to joint pain or fatigue, reduces natural stimulation of the digestive system. Sleep disturbances, another common menopause symptom, can disrupt the body's natural circadian rhythms that help regulate bowel movements.
Stress and mood changes during menopause can also impact digestive health through the gut-brain connection. Anxiety and depression, which affect many women during this transition, can alter gut bacteria and slow digestive processes.
Effective Dietary Strategies for Menopause-Related Constipation
Dietary modifications represent the first line of defense against constipation during menopause. Increasing fiber intake gradually can help restore regular bowel movements without causing uncomfortable bloating or gas.
Focus on incorporating both soluble and insoluble fiber sources. Soluble fiber, found in oats, beans, and fruits like apples and berries, helps soften stools by absorbing water. Insoluble fiber from vegetables, whole grains, and nuts adds bulk to stools and promotes movement through the digestive tract.
Hydration and Timing Considerations
Adequate hydration becomes even more critical during menopause, as the body's water retention capacity decreases with hormonal changes. Aim for at least 8-10 glasses of water daily, and consider starting each morning with a glass of warm water to stimulate digestive activity.
Meal timing also plays a role in managing constipation. Eating smaller, more frequent meals can be easier on the digestive system than three large meals. Try to establish regular meal times to help train your digestive system to follow a predictable schedule.
Lifestyle Modifications That Make a Difference
Regular physical activity serves as a natural stimulant for digestive function. Even moderate exercise like walking for 30 minutes daily can significantly improve bowel regularity. The physical movement helps massage internal organs and promotes healthy gut motility.
Yoga poses specifically targeting the abdominal area can be particularly beneficial. Gentle twisting poses, child's pose, and knees-to-chest positions can help stimulate the digestive tract and provide relief from constipation.
Stress Management and Sleep Hygiene
Managing stress through techniques like deep breathing, meditation, or gentle stretching can positively impact digestive health. The gut-brain connection means that reducing stress often translates to improved digestive function.
Establishing good sleep hygiene practices supports overall hormonal balance and digestive health. Aim for 7-9 hours of quality sleep nightly, and try to maintain consistent sleep and wake times to support your body's natural rhythms.
Medical Treatments and Natural Remedies
Several over-the-counter options can provide relief from menopause-related constipation. Bulk-forming laxatives containing psyllium husk or methylcellulose are generally safe for long-term use and work by adding fiber to the diet.
Stool softeners like docusate sodium can help when stools are particularly hard, while osmotic laxatives such as polyethylene glycol draw water into the intestines to soften stool consistency.
Natural Approaches and Supplements
Probiotics can help restore healthy gut bacteria balance, which may be disrupted during menopause. Look for supplements containing multiple strains of beneficial bacteria, particularly Lactobacillus and Bifidobacterium species.
Magnesium supplements serve dual purposes during menopause, potentially helping with both constipation and sleep issues. Start with a lower dose to avoid digestive upset, and consider magnesium glycinate for better absorption and fewer side effects.
The Role of Hormone Replacement Therapy
Hormone replacement therapy (HRT) can sometimes improve digestive symptoms by restoring hormonal balance. Some women find that HRT helps normalize their bowel movements along with addressing other menopause symptoms.
However, HRT isn't appropriate for everyone and may carry certain health risks. The decision to use hormone therapy should always be made in consultation with a healthcare provider who can evaluate individual risk factors and benefits.
For women who cannot use traditional HRT, bioidentical hormones or selective estrogen receptor modulators might be alternatives worth discussing with a healthcare professional.
Frequently Asked Questions
What causes constipation during menopause and how do hormonal changes affect digestion?
Constipation during menopause is primarily caused by declining estrogen and progesterone levels. These hormones help maintain healthy gut motility and digestive enzyme production. When they decrease, the digestive tract slows down, allowing more water to be absorbed from waste materials and resulting in harder, more difficult-to-pass stools. The reduction in smooth muscle contractions in the intestinal wall also contributes to slower transit times.
What are the most effective dietary and lifestyle changes to relieve constipation in menopausal women?
The most effective changes include gradually increasing fiber intake from both soluble and insoluble sources, drinking 8-10 glasses of water daily, and eating smaller, more frequent meals. Regular physical activity, even just 30 minutes of walking daily, can significantly improve bowel regularity. Establishing consistent meal and sleep schedules also helps train the digestive system to function more predictably.
Can hormone replacement therapy help improve constipation symptoms during menopause?
Hormone replacement therapy may help improve constipation symptoms by restoring hormonal balance and supporting normal digestive function. Some women experience improved bowel regularity along with relief from other menopause symptoms. However, HRT isn't suitable for everyone and carries potential health risks. The decision should be made individually with a healthcare provider after evaluating personal risk factors and benefits.
Which over-the-counter treatments and natural remedies are safe and effective for menopause-related constipation?
Safe over-the-counter options include bulk-forming laxatives with psyllium husk or methylcellulose, stool softeners like docusate sodium, and osmotic laxatives such as polyethylene glycol. Natural remedies include probiotic supplements to restore gut bacteria balance and magnesium supplements, which can help with both constipation and sleep issues. Always start with lower doses and consult a pharmacist or healthcare provider about interactions with other medications.
When should I see a doctor about constipation that occurs during or after menopause?
Consult a healthcare provider if constipation persists for more than two weeks despite dietary and lifestyle changes, if you experience severe abdominal pain or bloating, or if you notice blood in your stool. Also seek medical attention if constipation is accompanied by unexplained weight loss, severe cramping, or alternating constipation and diarrhea. Women with a family history of colorectal cancer or inflammatory bowel disease should discuss their symptoms with a doctor sooner rather than later.