Chronic Obstructive Pulmonary Disease (COPD) is a progressive respiratory condition that fundamentally changes how the lungs function. Understanding COPD pathophysiology is crucial for both healthcare providers and patients, as it helps explain why symptoms occur and how treatments work to manage the condition.
This comprehensive guide explores the complex mechanisms behind COPD, including how it affects lung structure and function, the role of inflammation, and the progressive nature of the disease.
The Basic Mechanisms of COPD
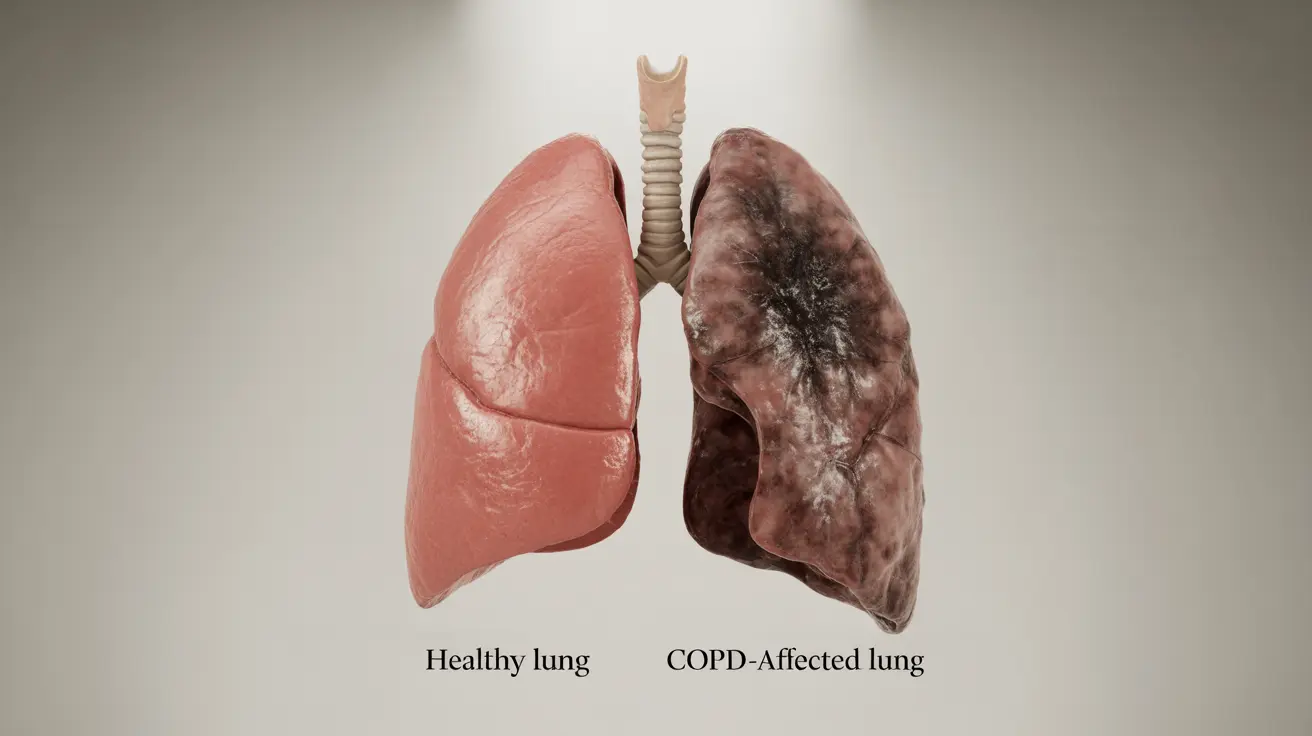
COPD pathophysiology involves several interconnected processes that affect the airways and lung tissue. The disease primarily impacts two crucial aspects of lung function: the airways (bronchi and bronchioles) and the air sacs (alveoli).
When COPD develops, three main changes occur in the lungs:
- Inflammation of the airways
- Destruction of lung tissue
- Excessive mucus production
Airway Changes and Inflammation
The airways undergo significant changes in COPD. Chronic inflammation causes the airway walls to thicken, while the smooth muscles surrounding them contract more readily. This combination leads to airway narrowing and increased resistance to airflow.
Understanding Emphysema and Chronic Bronchitis
COPD typically manifests as two main conditions: emphysema and chronic bronchitis. Though they often occur together, their pathophysiological processes differ significantly.
Emphysema's Impact
In emphysema, the walls between air sacs (alveoli) break down and lose their elasticity. This destruction results in fewer, larger air spaces instead of many small ones, reducing the surface area available for gas exchange. The loss of elastic recoil makes it particularly difficult to exhale effectively.
Chronic Bronchitis Mechanisms
Chronic bronchitis involves persistent inflammation of the bronchial tubes, leading to excessive mucus production and chronic cough. The airways become constantly inflamed and narrowed, making breathing increasingly difficult.
The Role of Inflammation in COPD
Inflammation plays a central role in COPD pathophysiology. When irritants like cigarette smoke enter the airways, they trigger an inflammatory response that, over time, becomes chronic and destructive. This ongoing inflammation leads to:
- Increased mucus production
- Tissue damage and remodeling
- Narrowing of airways
- Reduced lung elasticity
Disease Progression and Symptom Development
As COPD progresses, the combination of airway obstruction, tissue destruction, and chronic inflammation leads to increasingly severe symptoms. The body attempts to compensate for reduced lung function, but these adaptations often result in additional problems.
Impact on Daily Activities
The progressive nature of COPD means that activities requiring increased oxygen demand become increasingly difficult. This limitation occurs due to:
- Reduced oxygen absorption capability
- Increased work of breathing
- Air trapping in the lungs
- Muscle fatigue from increased respiratory effort
Frequently Asked Questions
What is the pathophysiology of COPD and how does it affect the lungs?
COPD pathophysiology involves chronic inflammation of airways, destruction of lung tissue, and excessive mucus production. These changes lead to narrowed airways, reduced elastic recoil, and decreased gas exchange capacity in the lungs.
How do emphysema and chronic bronchitis differ in their impact on COPD lung damage?
Emphysema primarily affects the air sacs (alveoli), causing their destruction and reducing surface area for gas exchange. Chronic bronchitis mainly impacts the airways, causing inflammation, mucus overproduction, and airway narrowing.
What causes inflammation and airflow obstruction in COPD?
Inflammation in COPD is primarily triggered by exposure to irritants, most commonly cigarette smoke. This leads to chronic inflammatory responses that cause airway wall thickening, increased mucus production, and tissue destruction.
How does COPD progression lead to symptoms like shortness of breath and mucus production?
As COPD progresses, the combination of airway narrowing, tissue destruction, and inflammation makes breathing increasingly difficult. Mucus production increases as a response to chronic irritation, while damaged air sacs and reduced elastic recoil contribute to shortness of breath.
What role does smoking play in the development and pathophysiology of COPD?
Smoking is the primary cause of COPD, triggering chronic inflammation and oxidative stress in the lungs. The toxic substances in cigarette smoke damage airway cells, destroy lung tissue, and impair the body's natural defense mechanisms against infection and injury.