Corneal edema is a serious eye condition that occurs when the cornea, the clear front surface of your eye, swells with excess fluid. This swelling can significantly impact your vision and requires prompt medical attention. Understanding this condition is crucial for early recognition and effective treatment.
Whether caused by underlying health conditions, eye surgery complications, or trauma, corneal edema can lead to vision problems ranging from mild blurriness to severe visual impairment. This comprehensive guide explores the causes, symptoms, diagnosis, and treatment options available for managing corneal edema.
Understanding the Cornea and Corneal Edema
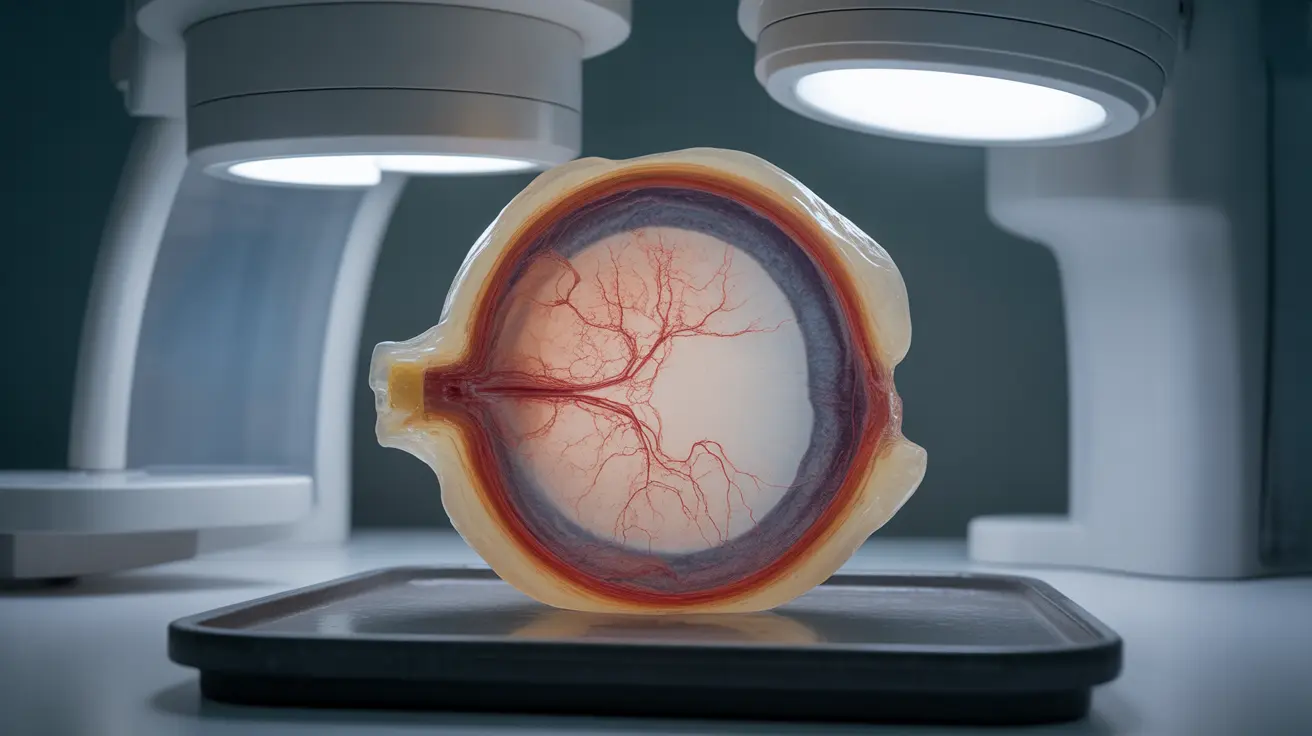
The cornea is a transparent, dome-shaped surface that covers the front of your eye. It plays a vital role in focusing light and protecting your eye's internal structures. When the cornea's delicate balance of fluid regulation is disrupted, swelling occurs, leading to corneal edema.
This condition develops when the cornea's endothelial cells, responsible for maintaining proper fluid levels, become damaged or dysfunction. As a result, excess fluid accumulates in the corneal tissue, causing it to become cloudy and swollen.
Common Causes and Risk Factors
Several factors can contribute to the development of corneal edema:
- Fuchs' dystrophy (an inherited condition)
- Cataract surgery complications
- Eye trauma or injury
- High intraocular pressure
- Viral infections
- Genetic predisposition
- Advanced age
- Previous eye surgeries
Recognizing the Symptoms
The symptoms of corneal edema can vary in severity and may include:
- Blurred or cloudy vision
- Light sensitivity
- Halos around lights
- Eye pain or discomfort
- Vision that's worse in the morning
- Feeling of pressure in the eye
- Reduced visual acuity
Diagnostic Process
Eye care professionals use several methods to diagnose corneal edema:
Visual Examination
Your doctor will perform a detailed examination using a slit lamp microscope to assess the cornea's thickness and clarity.
Specialized Testing
Additional tests may include:
- Pachymetry to measure corneal thickness
- Specular microscopy to evaluate endothelial cells
- Corneal topography to map the cornea's surface
- Visual acuity tests
Treatment Approaches
Treatment options for corneal edema range from conservative management to surgical intervention, depending on the severity and cause:
Conservative Management
- Hypertonic eye drops or ointments
- Dehydrating agents
- Protective eyewear
- Environmental modifications
Surgical Options
When conservative treatments aren't sufficient, surgical procedures may be necessary:
- DSEK (Descemet's Stripping Endothelial Keratoplasty)
- Full corneal transplant
- Amniotic membrane transplantation
Prevention and Management
While not all cases of corneal edema can be prevented, certain measures can help reduce risk and manage symptoms:
- Regular eye examinations
- Protecting eyes from injury
- Managing underlying health conditions
- Following post-operative care instructions carefully
- Maintaining good eye hygiene
Frequently Asked Questions
What causes corneal edema and how can I recognize its symptoms?
Corneal edema occurs when the cornea's endothelial cells fail to regulate fluid properly. Key symptoms include blurred vision, especially in the morning, light sensitivity, and a feeling of pressure in the eye.How is corneal edema diagnosed and what tests are involved?
Diagnosis involves a comprehensive eye examination using a slit lamp microscope, pachymetry to measure corneal thickness, and specular microscopy to evaluate endothelial cell health.What treatment options are available for managing corneal edema, including medications and surgery?
Treatment options range from hypertonic eye drops and ointments to surgical procedures like DSEK or full corneal transplantation, depending on the severity and cause of the condition.Can corneal edema caused by eye surgery or injury be prevented or minimized?
While not all cases can be prevented, following proper eye protection measures, maintaining good eye health, and carefully following post-operative instructions can help minimize risk.What should I expect during recovery from corneal edema surgery like DSEK or corneal transplant?
Recovery typically involves several weeks of healing, regular follow-up appointments, use of prescribed medications, and temporary activity restrictions. Full vision improvement may take several months.