Coughing up bloody mucus, also known as hemoptysis, can be an alarming symptom that requires careful medical attention. While this condition can range from mild to severe, understanding its causes and knowing when to seek immediate medical care is crucial for your health and safety.
This comprehensive guide will explore the various causes of bloody mucus, warning signs that indicate an emergency, diagnostic processes, and available treatments to help you better understand this concerning symptom.
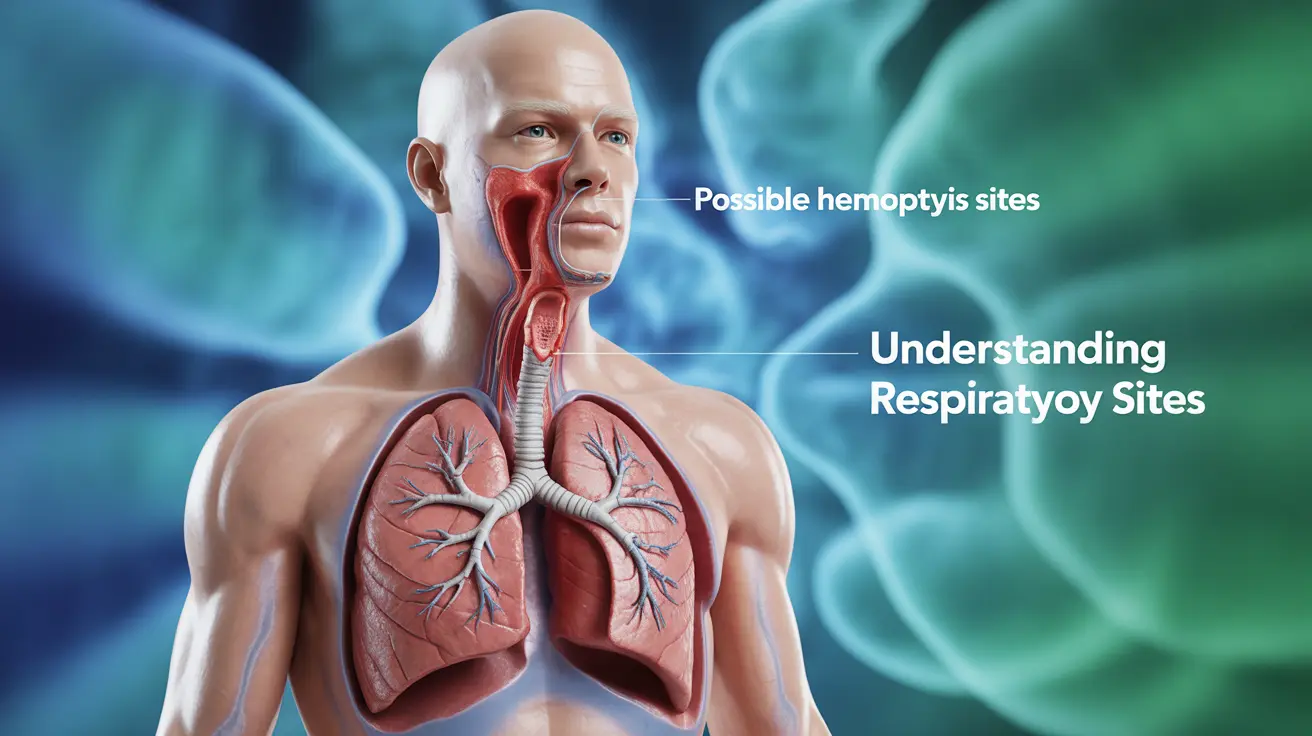
Understanding Bloody Mucus in Cough
When you cough up bloody mucus, it means blood is mixing with the sputum (mucus) from your respiratory tract. The blood can come from anywhere in your respiratory system, from your nose and throat to your lungs. The amount and appearance of blood can vary significantly, ranging from light pink streaks to bright red spots or darker, coffee-ground-like material.
Common Causes of Bloody Mucus
Several conditions can lead to coughing up bloody mucus, ranging from mild to serious:
Acute Conditions
- Bronchitis
- Pneumonia
- Upper respiratory infections
- Trauma to the airways
- Intense coughing episodes
Chronic Conditions
- Bronchiectasis
- Chronic bronchitis
- Cystic fibrosis
- Pulmonary embolism
- Tuberculosis
- Lung cancer
Warning Signs and Emergency Situations
While any instance of coughing up blood should be evaluated by a healthcare provider, certain situations require immediate emergency care:
- Coughing up more than a few teaspoons of blood
- Blood accompanied by severe shortness of breath
- Chest pain or tightness
- Dizziness or lightheadedness
- Fever above 101°F (38.3°C)
Diagnostic Process
Healthcare providers use various methods to determine the underlying cause of bloody mucus:
Physical Examination
- Vital signs assessment
- Lung sound evaluation
- Medical history review
Diagnostic Tests
- Chest X-ray
- CT scan
- Bronchoscopy
- Blood tests
- Sputum analysis
Treatment Approaches
Treatment for coughing up bloody mucus depends entirely on the underlying cause:
Conservative Management
- Rest and monitoring
- Humidification
- Cough suppressants (when appropriate)
- Smoking cessation
Medical Interventions
- Antibiotics for bacterial infections
- Anti-inflammatory medications
- Bronchodilators
- Specific treatments for identified conditions
Frequently Asked Questions
What are the common causes of coughing up bloody mucus?
Common causes include bronchitis, pneumonia, tuberculosis, bronchiectasis, and in some cases, lung cancer. Less severe causes might include intense coughing episodes or upper respiratory infections.
When should I seek emergency care if I cough up blood?
Seek immediate medical attention if you cough up more than a few teaspoons of blood, experience severe shortness of breath, chest pain, fever above 101°F, or feel dizzy. These symptoms could indicate a serious condition requiring urgent care.
How do doctors diagnose the cause of coughing up blood with mucus?
Doctors typically start with a physical examination and medical history review, followed by diagnostic tests such as chest X-rays, CT scans, bronchoscopy, blood tests, and sputum analysis to determine the underlying cause.
What treatments are available for hemoptysis (coughing up blood)?
Treatment options vary based on the underlying cause and may include antibiotics for infections, anti-inflammatory medications, bronchodilators, or specific treatments for identified conditions. Some cases may require conservative management with rest and monitoring.
Can coughing up bloody mucus be a sign of lung cancer or tuberculosis?
Yes, coughing up bloody mucus can be a symptom of both lung cancer and tuberculosis. While there are many other possible causes, these serious conditions should be ruled out by a healthcare provider, especially if accompanied by other symptoms like weight loss, persistent cough, or night sweats.