The relationship between COVID-19 and digestive symptoms has become increasingly clear as medical professionals gather more data about this viral infection. While respiratory symptoms often take center stage, many people experience gastrointestinal issues during and after COVID-19 infection, including constipation. Understanding this connection is crucial for both patients and healthcare providers.
This comprehensive guide explores the various ways COVID-19 can affect bowel movements, from direct viral impacts to indirect lifestyle changes during illness and recovery. We'll also discuss practical solutions and management strategies for COVID-related constipation.
The Direct Impact of COVID-19 on Digestive Function
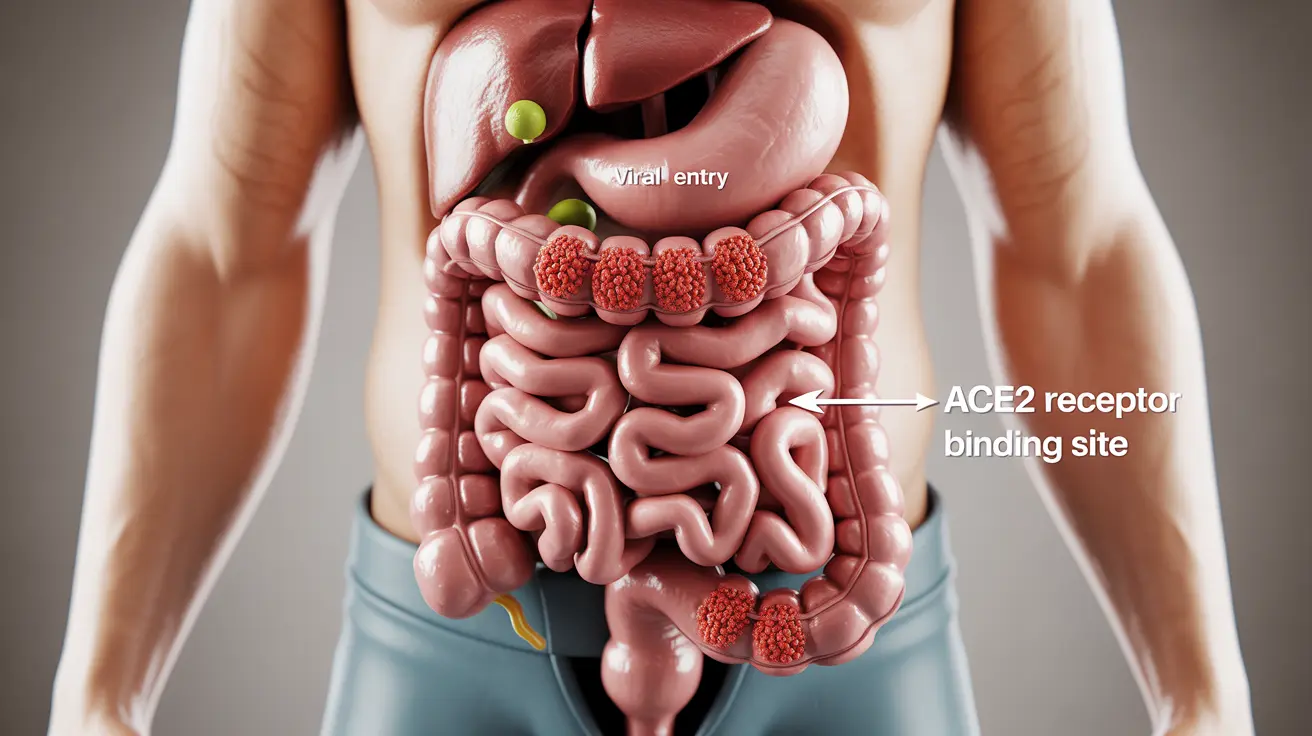
COVID-19 can directly affect the digestive system through several mechanisms. The virus has been shown to bind to ACE2 receptors, which are present throughout the gastrointestinal tract. This interaction can disrupt normal gut function and potentially lead to various digestive issues, including constipation.
Research indicates that the virus may temporarily alter gut motility and affect the nervous system controlling intestinal movement, potentially contributing to constipation in some patients.
Medication-Related Constipation During COVID-19
Many medications commonly used to treat COVID-19 symptoms can contribute to constipation as a side effect. These include:
- Pain relievers and fever reducers
- Some antiviral medications
- Certain supplements recommended during COVID-19 treatment
- Anti-nausea medications
Understanding these medication-related effects can help patients and healthcare providers better manage digestive health during COVID-19 treatment.
Lifestyle Factors During COVID-19 Recovery
Several lifestyle changes during COVID-19 illness and recovery can increase the risk of constipation:
- Reduced physical activity during isolation
- Changes in daily routine and eating habits
- Decreased fluid intake while managing fever
- Stress and anxiety related to illness
Prevention Strategies During Recovery
Taking proactive steps during COVID-19 recovery can help maintain regular bowel movements:
- Maintaining adequate hydration
- Incorporating gentle movement when possible
- Following a fiber-rich diet
- Establishing regular bathroom routines
Managing Long-Term Digestive Changes
Some individuals experience persistent digestive symptoms, including constipation, as part of long COVID. This may require ongoing management strategies and possibly professional medical support for optimal resolution.
Frequently Asked Questions
Can COVID-19 infection directly cause constipation as a symptom?
Yes, COVID-19 can directly cause constipation by affecting the gut's ACE2 receptors and disrupting normal digestive system function. The virus can impact gut motility and the nervous system controlling intestinal movement.
How do COVID-19 medications contribute to constipation?
Many medications used to treat COVID-19 symptoms, including pain relievers, antivirals, and certain supplements, can slow down digestive function as a side effect. This medication-induced constipation is typically temporary and resolves after discontinuing the medications.
What lifestyle changes during the COVID-19 pandemic increase the risk of constipation?
Reduced physical activity, changes in diet and daily routine, decreased fluid intake, and increased stress levels during illness can all contribute to constipation. These factors often combine to affect normal bowel habits.
How long can constipation last after recovering from COVID-19 or in long COVID cases?
The duration of constipation can vary significantly among individuals. Some people experience temporary symptoms that resolve within weeks, while others with long COVID may have persistent digestive issues lasting months. Professional medical evaluation is recommended for prolonged symptoms.
What are effective ways to manage or prevent constipation related to COVID-19 or its aftermath?
Effective management strategies include maintaining proper hydration, eating a fiber-rich diet, engaging in gentle physical activity when possible, and establishing regular bathroom routines. Some people may benefit from over-the-counter remedies, but should consult healthcare providers before use.