As COVID-19 vaccines continue to play a crucial role in fighting the pandemic, questions have emerged about their relationship with other health conditions, particularly shingles (herpes zoster). This comprehensive guide examines the connection between COVID-19 vaccination and shingles risk, helping you understand what the current medical evidence shows.
Whether you're planning to get vaccinated or have already received your COVID-19 shots, it's important to understand the facts about potential side effects and interactions with other conditions like shingles.
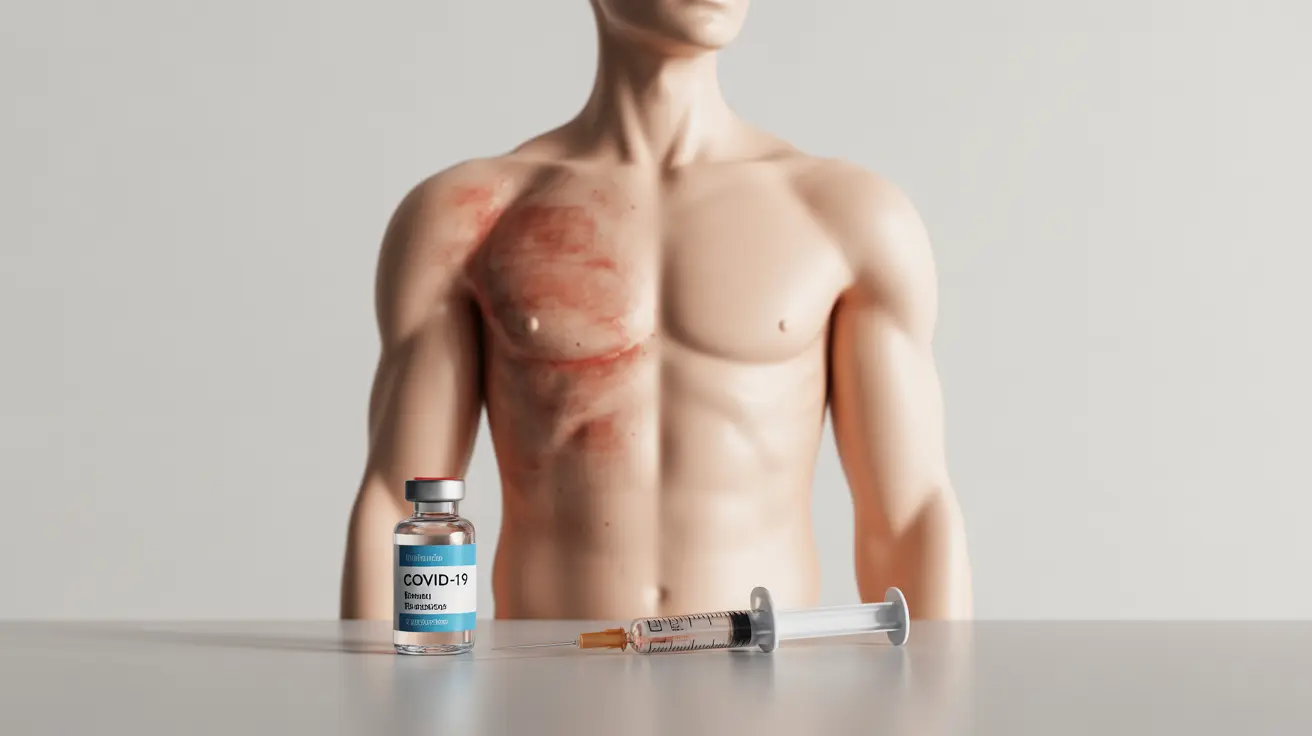
The Link Between COVID-19 Vaccines and Shingles
Research has shown that while there may be a small number of reported cases of shingles following COVID-19 vaccination, this doesn't necessarily indicate a direct causal relationship. The occurrence of shingles after vaccination appears to be rare and may be related to the temporary effects that vaccines can have on the immune system.
It's important to note that shingles cases have been reported following various types of vaccinations, not just COVID-19 vaccines, suggesting this isn't unique to COVID-19 vaccination.
Understanding Your Risk Factors
Several factors can influence your risk of developing shingles, whether or not you receive a COVID-19 vaccine:
- Age (50 years and older)
- Weakened immune system
- History of chickenpox
- Chronic stress
- Certain medications that affect immune function
These underlying risk factors are often more significant determinants of shingles occurrence than vaccination status.
Recognizing Shingles Symptoms
If you develop shingles after receiving a COVID-19 vaccine, the symptoms are the same as in any other case of shingles:
- Painful rash that typically appears on one side of the body
- Burning, tingling, or numbness
- Blisters that fill with fluid and then crust over
- Itching
- Sensitivity to touch
Early recognition and treatment of these symptoms can help manage the condition more effectively.
Treatment and Management
If you develop shingles after receiving a COVID-19 vaccine, standard treatment protocols apply:
- Antiviral medications (most effective when started within 72 hours)
- Pain management medications
- Topical treatments for skin discomfort
- Rest and stress reduction
- Keeping the rash clean and covered
Vaccination Timing Considerations
For those concerned about both COVID-19 and shingles prevention, current medical guidelines support receiving both vaccines when needed. However, it's important to discuss optimal timing with your healthcare provider based on your individual circumstances.
Frequently Asked Questions
Can the COVID-19 vaccine cause shingles or trigger a shingles outbreak?
While there have been some reported cases of shingles following COVID-19 vaccination, current evidence doesn't suggest that the vaccine directly causes shingles. Any potential relationship appears to be rare and may be related to temporary immune system changes that can occur with any vaccination.
Who is at higher risk of developing shingles after receiving a COVID-19 vaccine?
People who are older (50+), have weakened immune systems, or have a history of shingles may be at higher risk. However, these are the same risk factors for shingles in general, regardless of COVID-19 vaccination status.
Is it safe to get the shingles vaccine (Shingrix) at the same time as the COVID-19 vaccine?
Current CDC guidelines indicate that it is generally safe to receive both vaccines. However, individual circumstances may vary, and you should consult with your healthcare provider about optimal timing for your situation.
What are the symptoms of shingles and how is it treated if it occurs after COVID-19 vaccination?
Symptoms include a painful rash, typically on one side of the body, along with burning, tingling, and blisters. Treatment remains the same whether or not it occurs after vaccination: antiviral medications, pain management, and supportive care.
Does receiving a COVID-19 vaccine increase my overall risk of getting shingles compared to not being vaccinated?
Current evidence doesn't suggest that COVID-19 vaccination significantly increases overall shingles risk. The baseline risk of shingles is more strongly influenced by factors such as age, immune status, and history of chickenpox.