Living with diabetes can present various challenges, and one particularly troublesome complication is diabetic diarrhea. This condition can significantly impact quality of life and requires careful management through multiple approaches. Understanding how to effectively treat and control diabetic diarrhea is crucial for maintaining overall health and well-being.
In this comprehensive guide, we'll explore various treatment options, lifestyle modifications, and medical interventions that can help manage and potentially cure diabetic diarrhea. We'll also discuss the important connection between blood sugar control and digestive health.
Understanding Diabetic Diarrhea and Its Causes
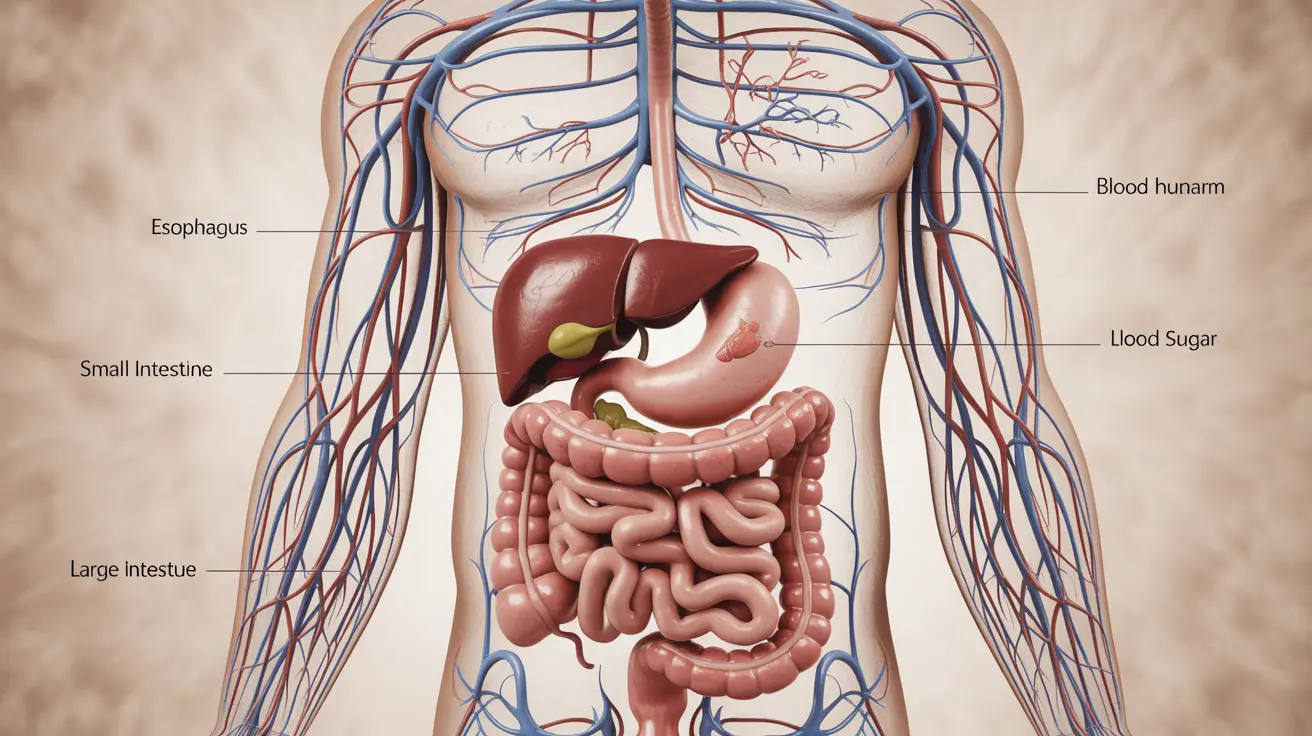
Diabetic diarrhea occurs as a result of several factors, including autonomic neuropathy, which affects nerve function in the digestive system. This condition can lead to irregular bowel movements and poor control over digestive processes. Additionally, bacterial overgrowth and medication side effects can contribute to persistent diarrhea in diabetic patients.
Blood Sugar Control and Digestive Health
Maintaining stable blood sugar levels is fundamental in managing diabetic diarrhea. High blood glucose can damage nerves throughout the body, including those controlling digestive function. By keeping blood sugar within target ranges, you can help prevent further nerve damage and potentially improve existing symptoms.
Strategies for Blood Sugar Management
To maintain optimal blood sugar levels:
- Regular blood glucose monitoring
- Consistent medication schedule
- Balanced meal planning
- Regular physical activity
- Stress management techniques
Medical Treatments for Diabetic Diarrhea
Several medical interventions can help manage diabetic diarrhea effectively. These may include:
- Anti-diarrheal medications
- Antibiotics for bacterial overgrowth
- Prescription medications for nerve pain
- Probiotics to restore gut balance
Managing Medication-Related Diarrhea
Some diabetes medications, particularly metformin, can cause diarrhea as a side effect. Working with your healthcare provider to adjust dosage or timing of medication can help minimize these effects. In some cases, extended-release formulations may be recommended.
Dietary Modifications and Lifestyle Changes
Making strategic dietary changes can significantly impact diabetic diarrhea symptoms:
- Increase soluble fiber intake gradually
- Stay well-hydrated with water and sugar-free beverages
- Avoid caffeine and alcohol
- Identify and eliminate trigger foods
- Eat smaller, more frequent meals
Hydration and Electrolyte Balance
Maintaining proper hydration is crucial when dealing with diabetic diarrhea. Focus on replacing lost fluids and electrolytes through:
- Regular water intake
- Sugar-free electrolyte solutions
- Clear broths
- Herbal teas
When to Seek Medical Attention
It's important to know when professional medical help is necessary. Contact your healthcare provider if you experience:
- Severe or persistent diarrhea
- Signs of dehydration
- Unexplained weight loss
- Blood in stool
- Severe abdominal pain
Frequently Asked Questions
What are the most effective treatments to manage and reduce diabetic diarrhea symptoms? The most effective treatments include maintaining stable blood sugar levels, taking prescribed anti-diarrheal medications, following a proper diet plan, and staying well-hydrated. Some patients may also benefit from probiotics and specific medications to address nerve damage.
How does controlling blood sugar levels help in curing or improving diabetic diarrhea? Stable blood sugar levels help prevent further nerve damage and can improve existing symptoms by reducing inflammation and supporting proper nerve function in the digestive system. Good glycemic control is essential for long-term management of diabetic diarrhea.
Can diabetic medications like metformin cause or worsen diarrhea, and how can this be managed? Yes, metformin and some other diabetes medications can cause diarrhea. This can be managed by taking medication with meals, using extended-release formulations, or adjusting dosage under medical supervision. Never modify medication schedules without consulting your healthcare provider.
What dietary changes can help ease diabetic diarrhea and prevent dehydration? Key dietary changes include increasing soluble fiber intake gradually, avoiding trigger foods, eating smaller meals more frequently, and ensuring adequate hydration with water and sugar-free beverages. Following a balanced diet that supports stable blood sugar is also crucial.
When should I see a doctor for persistent or severe diabetic diarrhea, and what tests or treatments might they recommend? Seek medical attention if diarrhea persists for more than a few days, causes dehydration, or is accompanied by severe pain or bleeding. Doctors may recommend tests like stool analysis, endoscopy, or autonomic function tests, and may prescribe specific medications based on the underlying cause.