Living with cystic fibrosis (CF) significantly impacts lung health and respiratory function. Understanding the distinct differences between CF-affected lungs and healthy lungs helps patients, families, and caregivers better manage this challenging genetic condition and its effects on breathing and quality of life.
This comprehensive guide explores how cystic fibrosis alters lung structure and function, leading to unique challenges in breathing and respiratory health. We'll examine the key differences, complications, and modern treatment approaches that help CF patients maintain optimal lung function.
The Basic Structure: CF Lungs vs. Healthy Lungs
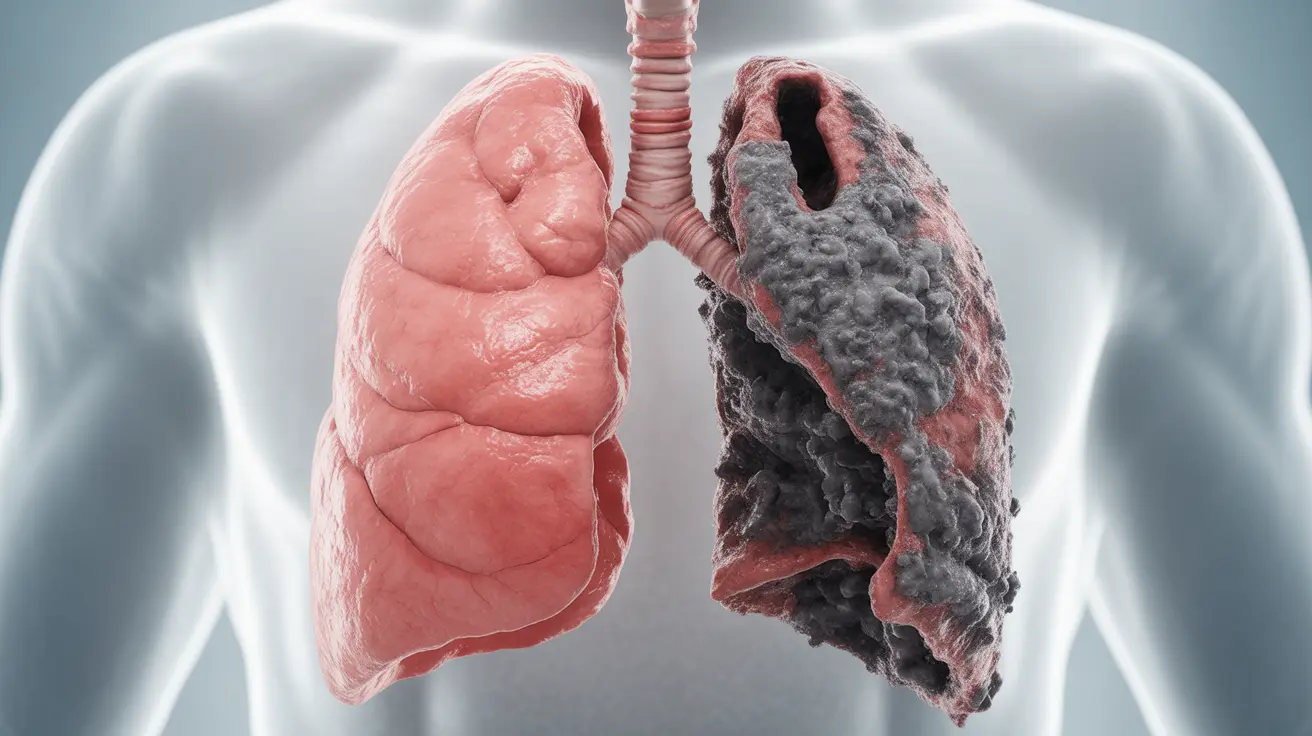
In healthy lungs, the airways are lined with a thin layer of mucus that helps trap particles and bacteria while allowing easy air movement. However, in CF lungs, a defective gene causes significant changes to this normal structure:
- Thick, sticky mucus accumulation
- Narrowed airways
- Inflammation of the bronchial walls
- Reduced ability to clear bacteria and particles
These structural differences create the foundation for many of the breathing challenges experienced by CF patients.
How CF Affects Lung Function
The primary difference between CF lungs and healthy lungs lies in how they handle mucus production and clearance. In CF, the CFTR gene mutation affects how cells process chloride, leading to:
- Dehydrated airway surfaces
- Abnormally thick mucus secretions
- Impaired mucociliary clearance
- Increased risk of bacterial colonization
These alterations significantly impact the lungs' ability to function normally and protect against infections.
Common Respiratory Complications
The unique characteristics of CF lungs often lead to several respiratory complications:
Chronic Infections
Thick mucus creates an ideal environment for bacterial growth, leading to frequent lung infections. Common pathogens include Pseudomonas aeruginosa and Staphylococcus aureus.
Bronchiectasis
Repeated infections and inflammation can cause permanent airway damage, resulting in bronchiectasis - a condition where airways become abnormally widened and scarred.
Respiratory Insufficiency
Over time, ongoing damage to the airways can lead to decreased lung function and respiratory insufficiency, making breathing increasingly difficult.
Modern Treatment Approaches
While CF lung damage cannot be completely reversed, several treatment strategies help manage symptoms and slow disease progression:
Airway Clearance Techniques
- Chest physical therapy
- Oscillating devices
- High-frequency chest wall oscillation
- Exercise-based clearance methods
Medication Management
- Inhaled antibiotics
- Mucolytics to thin secretions
- Anti-inflammatory drugs
- CFTR modulators
Frequently Asked Questions
What is the main difference between healthy lungs and those affected by cystic fibrosis?
The key difference lies in mucus production and consistency. CF lungs produce thick, sticky mucus that's difficult to clear, while healthy lungs produce thin mucus that's easily expelled. This difference affects breathing and infection risk.
How does cystic fibrosis cause chronic lung infections and breathing problems?
CF causes thick mucus accumulation in the airways, creating an ideal environment for bacterial growth. This mucus is difficult to clear, leading to chronic infections, inflammation, and breathing difficulties.
What are the most common symptoms and complications of cystic fibrosis in the lungs?
Common symptoms include persistent coughing, frequent lung infections, shortness of breath, and reduced exercise tolerance. Complications can include bronchiectasis, respiratory failure, and chronic bacterial colonization.
What treatments and therapies help manage lung symptoms in cystic fibrosis?
Treatment typically involves a combination of airway clearance techniques, medications (including antibiotics and mucolytics), CFTR modulators, and regular exercise. Physical therapy and proper nutrition also play crucial roles.
Can lung damage from cystic fibrosis be reversed, and what are the long-term outlooks for patients?
While structural lung damage cannot be fully reversed, modern treatments can help slow disease progression and improve quality of life. Early intervention and consistent treatment adherence are crucial for better long-term outcomes. Life expectancy has significantly improved with modern therapies.