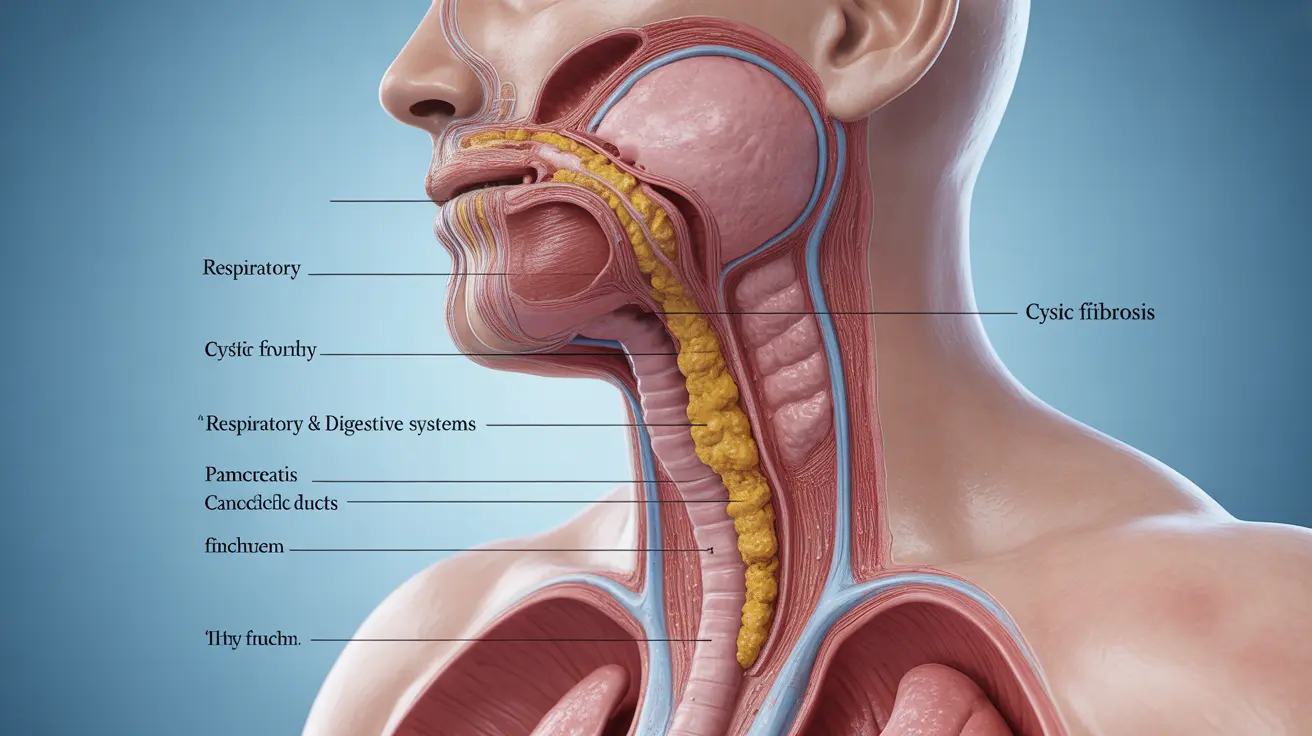
Cystic fibrosis is a serious genetic disorder that affects thousands of individuals worldwide, causing significant challenges to the respiratory and digestive systems. This inherited condition occurs when a person receives two defective copies of the CFTR gene, leading to the production of thick, sticky mucus that can clog airways and block digestive enzymes.
Understanding cystic fibrosis is crucial for families, healthcare providers, and communities, as early recognition and proper management can dramatically improve quality of life and outcomes for those affected by this condition.
What Is Cystic Fibrosis?
Cystic fibrosis is an autosomal recessive genetic disorder that primarily impacts the lungs, pancreas, liver, kidneys, and intestines. The condition results from mutations in the CFTR (Cystic Fibrosis Transmembrane Conductance Regulator) gene, which normally helps regulate the movement of salt and water in and out of cells.
When this gene is faulty, it produces abnormally thick and sticky secretions that can obstruct various organ systems. This leads to chronic infections, inflammation, and progressive damage to affected organs, particularly the lungs and digestive system.
Recognizing the Signs and Symptoms
Respiratory Symptoms
The most prominent symptoms of cystic fibrosis affect the respiratory system. Individuals with this condition often experience persistent coughing that produces thick, sticky mucus. This cough may worsen over time and can be accompanied by wheezing, shortness of breath, and repeated lung infections.
Sinus infections are also common, as the thick secretions can block nasal passages and create an environment conducive to bacterial growth. Many people with cystic fibrosis develop nasal polyps, which are small, benign growths that can further obstruct breathing.
Digestive Complications
Cystic fibrosis significantly impacts the digestive system by blocking the release of digestive enzymes from the pancreas. This leads to malabsorption of nutrients, particularly fats and fat-soluble vitamins. As a result, individuals may experience frequent, bulky, greasy stools that have a strong odor.
Poor weight gain despite a good appetite is another hallmark sign, especially in children. The inability to properly digest and absorb nutrients can lead to failure to thrive in infants and children, making early diagnosis and intervention critical.
Additional Manifestations
Other symptoms may include salty-tasting skin, which occurs due to increased salt content in sweat. Some individuals develop intestinal blockages, and men with cystic fibrosis are often infertile due to absent or blocked vas deferens.
Diagnostic Approaches and Testing Methods
Newborn Screening Programs
Most states in the United States now include cystic fibrosis screening as part of routine newborn testing. This screening involves analyzing a small blood sample, typically collected via a heel stick, to measure levels of immunoreactive trypsinogen (IRT), an enzyme produced by the pancreas.
Elevated IRT levels may indicate cystic fibrosis, prompting further testing. However, it's important to note that not all babies with elevated IRT levels have cystic fibrosis, and additional confirmatory tests are necessary.
Confirmatory Testing
The gold standard for diagnosing cystic fibrosis remains the sweat chloride test. This non-invasive procedure measures the amount of chloride in sweat, as people with cystic fibrosis have significantly higher chloride levels than normal.
Genetic testing can also confirm the diagnosis by identifying specific mutations in the CFTR gene. This type of testing is particularly useful when sweat test results are inconclusive or when there's a family history of the condition.
Additional Diagnostic Tools
Healthcare providers may also use pulmonary function tests to assess lung capacity and function, chest X-rays to detect lung changes, and stool tests to check for digestive enzyme deficiencies. These tests help create a comprehensive picture of how cystic fibrosis is affecting an individual's health.
Treatment Strategies and Management Options
Airway Clearance Therapies
Managing cystic fibrosis requires a comprehensive approach that addresses both respiratory and digestive symptoms. Airway clearance techniques are fundamental to treatment, helping to loosen and remove thick mucus from the lungs. These may include chest physiotherapy, oscillating positive expiratory pressure devices, and high-frequency chest wall oscillation vests.
Inhaled medications play a crucial role in treatment, including bronchodilators to open airways, mucolytics to thin secretions, and inhaled antibiotics to combat chronic bacterial infections. Many patients require regular use of these medications as part of their daily routine.
Nutritional Support and Enzyme Replacement
Since pancreatic enzyme deficiency is common in cystic fibrosis, most patients require pancreatic enzyme replacement therapy (PERT) with meals and snacks. These enzymes help break down fats, proteins, and carbohydrates, improving nutrient absorption and supporting proper growth and development.
Fat-soluble vitamin supplements (A, D, E, and K) are typically necessary, as these vitamins are poorly absorbed without adequate enzyme function. High-calorie, high-fat diets are often recommended to meet increased nutritional needs.
Advanced Therapeutic Options
Recent advances in cystic fibrosis treatment include CFTR modulators, medications that target the underlying protein defect. These drugs can improve CFTR protein function in people with specific genetic mutations, offering hope for better long-term outcomes.
For individuals with severe lung disease, lung transplantation may be considered as a treatment option. Physical therapy and exercise programs are also important components of comprehensive care, helping to maintain lung function and overall fitness.
Prognosis and Life Expectancy Considerations
The outlook for people with cystic fibrosis has improved dramatically over the past several decades due to advances in early diagnosis, comprehensive care, and new treatment options. While cystic fibrosis remains a serious condition, many individuals now live well into adulthood and can pursue education, careers, and relationships.
Factors that influence prognosis include the specific genetic mutations present, how early treatment begins, access to specialized care, and individual response to therapy. Regular monitoring and preventive care are essential for maintaining health and preventing complications.
The development of precision medicine approaches, including gene therapy and advanced CFTR modulators, continues to offer hope for even better outcomes in the future. Ongoing research focuses on addressing the root causes of cystic fibrosis rather than just managing symptoms.
Frequently Asked Questions
What are the common symptoms of cystic fibrosis to look out for in children and adults?
Common symptoms include persistent coughing with thick, sticky mucus, frequent lung infections, wheezing, salty-tasting skin, poor weight gain despite good appetite, and bulky, greasy stools. In children, failure to thrive and recurrent sinus infections are often early warning signs. Adults may experience progressive lung disease, digestive problems, and fertility issues.
How is cystic fibrosis diagnosed through newborn screening and other tests?
Newborn screening involves testing a blood sample for elevated immunoreactive trypsinogen (IRT) levels. If screening suggests cystic fibrosis, confirmatory testing includes the sweat chloride test, which measures chloride levels in sweat, and genetic testing to identify CFTR gene mutations. Additional tests may include pulmonary function tests and stool analysis.
What treatments and therapies are available to manage cystic fibrosis symptoms?
Treatment includes airway clearance techniques, inhaled medications (bronchodilators, mucolytics, antibiotics), pancreatic enzyme replacement therapy, nutritional supplements, and CFTR modulator drugs for eligible patients. Physical therapy, exercise programs, and in severe cases, lung transplantation may also be part of the treatment plan.
How does cystic fibrosis affect nutrition and what dietary changes can help?
Cystic fibrosis impairs pancreatic enzyme production, leading to poor absorption of fats and nutrients. Patients typically need pancreatic enzyme supplements with meals, high-calorie and high-fat diets, fat-soluble vitamin supplements (A, D, E, K), and increased salt intake. Working with a dietitian specializing in cystic fibrosis is highly recommended.
What is the life expectancy for people living with cystic fibrosis today?
Life expectancy has significantly improved, with many people now living into their 40s, 50s, and beyond. The median survival age continues to increase due to early diagnosis, improved treatments, and comprehensive care. Individual outcomes vary based on genetic factors, early intervention, access to specialized care, and response to treatment.