The relationship between dehydration and overactive bladder (OAB) is complex and often misunderstood. While many people with overactive bladder might be tempted to reduce their fluid intake to manage frequent urination, this approach can actually worsen their condition and lead to additional complications.
Understanding how dehydration affects bladder function is crucial for developing effective management strategies for overactive bladder symptoms. This article explores the connection between dehydration and OAB, and provides evidence-based guidance for proper hydration management.
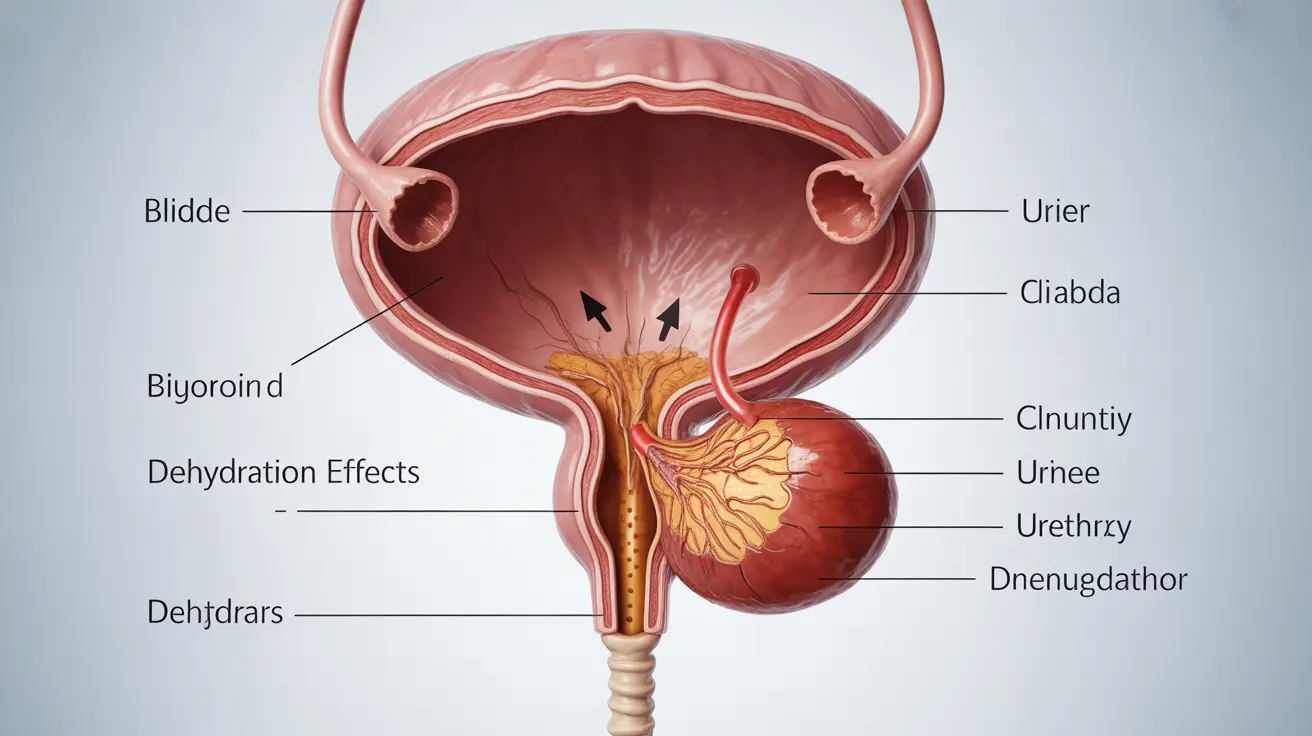
The Impact of Dehydration on Bladder Health
When you become dehydrated, your body produces more concentrated urine, which can irritate the bladder lining. This irritation may trigger or worsen overactive bladder symptoms, creating a cycle of increased urgency and frequency of urination despite having less fluid in your system.
The concentrated urine contains higher levels of waste products and minerals, which can act as irritants to the sensitive bladder tissue. This irritation can cause the bladder muscles to contract more frequently, leading to the characteristic symptoms of overactive bladder.
Understanding Proper Hydration for OAB Management
Managing fluid intake is a delicate balance for people with overactive bladder. While avoiding dehydration is essential, drinking too much can also exacerbate symptoms. The key is to maintain consistent, moderate fluid intake throughout the day.
Recommended Fluid Intake Guidelines
Most healthcare providers recommend the following approach to hydration for OAB patients:
- Aim for 6-8 glasses of water daily, spread evenly throughout the day
- Reduce fluid intake 2-3 hours before bedtime
- Monitor urine color (pale yellow indicates proper hydration)
- Adjust intake based on activity level and climate
Complications of Dehydration in OAB Patients
Chronic dehydration can lead to several complications for individuals with overactive bladder:
- Increased risk of urinary tract infections
- Kidney stone formation
- Bladder tissue irritation and inflammation
- Constipation, which can worsen OAB symptoms
- Concentrated urine leading to increased urgency
Lifestyle Modifications for Better Bladder Health
Managing overactive bladder requires a comprehensive approach that goes beyond just monitoring fluid intake. Consider these additional lifestyle modifications:
- Maintain a bladder diary to track fluid intake and urination patterns
- Avoid bladder irritants such as caffeine and alcohol
- Practice pelvic floor exercises
- Follow a consistent bathroom schedule
- Wear comfortable, loose-fitting clothing
Frequently Asked Questions
- Can dehydration cause or worsen symptoms of overactive bladder?
Yes, dehydration can worsen overactive bladder symptoms by producing concentrated urine that irritates the bladder lining, leading to increased urgency and frequency of urination. Proper hydration is essential for managing OAB symptoms effectively.
- How does concentrated urine from dehydration irritate the bladder in overactive bladder patients?
Concentrated urine contains higher levels of waste products and minerals that can irritate the sensitive bladder tissue, causing the bladder muscles to contract more frequently and triggering OAB symptoms.
- What are the best ways to manage fluid intake to reduce overactive bladder symptoms?
The best approach is to maintain consistent, moderate fluid intake throughout the day, aiming for 6-8 glasses of water, while reducing intake before bedtime. Monitor urine color and adjust intake based on activity level and climate.
- Can dehydration lead to urinary tract infections or other complications in people with overactive bladder?
Yes, dehydration can increase the risk of urinary tract infections, kidney stones, and bladder irritation in people with overactive bladder. Maintaining proper hydration helps prevent these complications.
- What lifestyle changes, including hydration habits, help prevent worsening of overactive bladder symptoms?
Key lifestyle changes include maintaining proper hydration, avoiding bladder irritants, practicing pelvic floor exercises, following a consistent bathroom schedule, and keeping a bladder diary to track patterns and triggers.