Brain fog—that frustrating experience of mental cloudiness, difficulty concentrating, and feeling like your thoughts are moving through molasses—affects millions of people worldwide. When you're struggling with depression, this cognitive haze can become an overwhelming daily reality that significantly impacts your quality of life.
The relationship between depression and brain fog is complex and bidirectional, with each condition potentially influencing and worsening the other. Understanding this connection is crucial for anyone experiencing these challenging symptoms and seeking effective treatment approaches.
The Science Behind Depression and Brain Fog
Depression fundamentally alters brain chemistry and function, creating an environment where cognitive symptoms like brain fog can flourish. Research shows that depression affects neurotransmitter systems, particularly serotonin, dopamine, and norepinephrine, which play essential roles in cognitive processing, attention, and mental clarity.
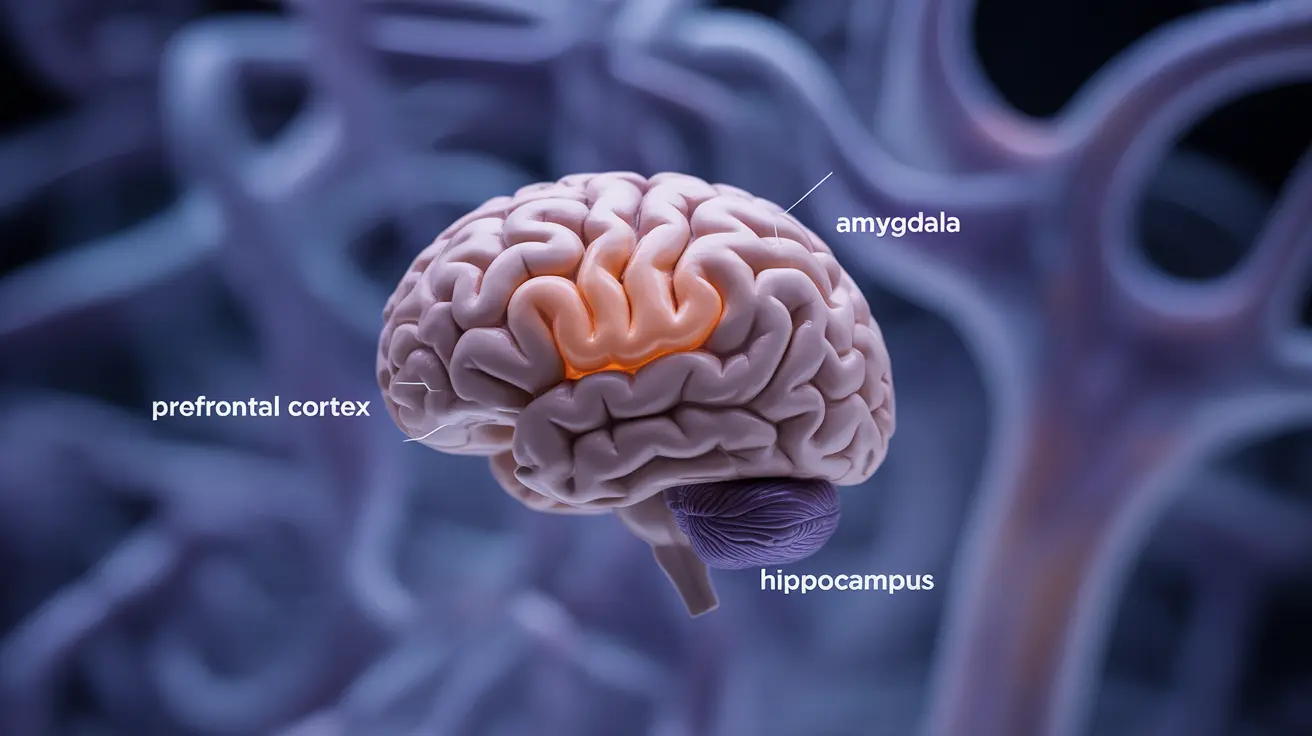
The prefrontal cortex, responsible for executive functions like decision-making and working memory, often shows decreased activity in people with depression. This reduction in neural efficiency directly contributes to the mental cloudiness that characterizes brain fog.
Chronic inflammation, commonly associated with depression, also impacts cognitive function. Inflammatory cytokines can cross the blood-brain barrier and interfere with normal brain processes, leading to difficulties with concentration, memory formation, and mental processing speed.
Common Symptoms of Depression-Related Brain Fog
Brain fog manifests differently for each individual, but several key symptoms frequently appear together with depression:
- Difficulty concentrating on tasks or conversations
- Problems with short-term and working memory
- Mental fatigue that doesn't improve with rest
- Trouble finding the right words during conversations
- Feeling mentally "sluggish" or slow to process information
- Difficulty making decisions, even simple ones
- Problems with multitasking or organizing thoughts
- Reduced mental clarity and sharpness
These cognitive symptoms often fluctuate in intensity, sometimes improving slightly during better mood periods but returning as depressive symptoms worsen.
Impact on Memory and Decision-Making
Depression-related brain fog significantly affects three core cognitive areas: memory formation and retrieval, concentration abilities, and decision-making processes. These interconnected functions rely on healthy neurotransmitter activity and efficient neural communication.
Memory Challenges
Working memory—your ability to hold and manipulate information temporarily—becomes compromised during depressive episodes. You might find yourself forgetting conversations from earlier in the day, struggling to remember appointments, or having difficulty retaining information while reading.
Long-term memory formation also suffers, as the emotional and cognitive burden of depression interferes with the brain's natural memory consolidation processes during sleep and rest periods.
Concentration Difficulties
Sustained attention becomes increasingly challenging when depression and brain fog coexist. Simple tasks that once required minimal effort—like reading emails, following television programs, or engaging in conversations—may demand significant mental energy and still result in incomplete comprehension.
Decision-Making Impairment
The combination of depression and brain fog creates a perfect storm for decision-making difficulties. Even routine choices like selecting what to wear or eat can feel overwhelming, while more complex decisions may seem impossible to navigate effectively.
Medication Considerations and Treatment Options
While antidepressant medications can be highly effective for treating depression, some individuals experience cognitive side effects that may initially worsen brain fog symptoms. This temporary increase in mental cloudiness typically occurs during the first few weeks of treatment as your brain adjusts to medication changes.
Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) generally have fewer cognitive side effects compared to older antidepressant classes. However, individual responses vary significantly, and working closely with your healthcare provider to find the right medication and dosage is essential.
Treatment Approaches for Cognitive Symptoms
Comprehensive treatment for depression-related brain fog often involves multiple therapeutic strategies:
- Cognitive behavioral therapy (CBT) to address both depressive thoughts and cognitive concerns
- Mindfulness-based interventions to improve present-moment awareness and attention
- Cognitive rehabilitation exercises to strengthen memory and concentration skills
- Medication optimization to balance mood improvement with minimal cognitive side effects
- Treatment of underlying sleep disorders or other medical conditions contributing to brain fog
Lifestyle Changes for Brain Fog Relief
Several evidence-based lifestyle modifications can significantly improve cognitive symptoms associated with depression:
Sleep Optimization
Quality sleep is fundamental for cognitive function and emotional regulation. Establishing consistent sleep schedules, creating optimal sleep environments, and addressing sleep disorders can dramatically improve brain fog symptoms.
Regular Physical Exercise
Aerobic exercise increases brain-derived neurotrophic factor (BDNF), promotes neuroplasticity, and enhances cognitive function. Even moderate activities like walking, swimming, or cycling can provide substantial cognitive benefits.
Nutritional Support
A balanced diet rich in omega-3 fatty acids, antioxidants, and B vitamins supports optimal brain function. Limiting processed foods, excessive sugar, and alcohol while maintaining stable blood sugar levels can reduce brain fog intensity.
Stress Management
Chronic stress exacerbates both depression and cognitive symptoms. Techniques such as meditation, deep breathing exercises, progressive muscle relaxation, and yoga can help reduce stress-related brain fog.
Social Engagement
Maintaining meaningful social connections provides cognitive stimulation and emotional support, both crucial for managing depression-related brain fog effectively.
Recovery Timeline and Prognosis
The duration of brain fog symptoms varies considerably among individuals and depends on multiple factors including depression severity, treatment adherence, underlying health conditions, and lifestyle factors. Understanding realistic timelines can help set appropriate expectations during recovery.
With effective depression treatment, many people begin experiencing cognitive improvements within 4-8 weeks, though complete resolution may take several months. Some individuals notice brain fog symptoms persisting even after mood symptoms improve, indicating the need for targeted cognitive interventions.
During remission periods, cognitive function typically continues improving gradually. However, maintaining treatment consistency and healthy lifestyle habits is crucial for preventing symptom recurrence and supporting long-term cognitive health.
Frequently Asked Questions
Does depression cause brain fog and what are the common symptoms associated with it?
Yes, depression commonly causes brain fog through alterations in brain chemistry, neurotransmitter function, and neural connectivity. Common symptoms include difficulty concentrating, memory problems, mental fatigue, trouble finding words, slowed thinking, decision-making difficulties, and reduced mental clarity. These cognitive symptoms often fluctuate alongside mood symptoms and can significantly impact daily functioning.
How does brain fog from depression affect memory, concentration, and decision-making?
Depression-related brain fog impairs working memory by making it difficult to hold and manipulate information temporarily. Concentration suffers as sustained attention becomes challenging, making simple tasks feel overwhelming. Decision-making abilities are compromised because the cognitive load required to evaluate options and consequences becomes exhausting, leading to difficulty with both routine and complex choices.
Can antidepressant medications make brain fog worse, and what treatment options help cognitive symptoms in depression?
Some antidepressant medications may temporarily worsen brain fog during the initial adjustment period, typically lasting 2-4 weeks. However, SSRIs and SNRIs generally have fewer cognitive side effects than older medication classes. Treatment options for cognitive symptoms include cognitive behavioral therapy, mindfulness interventions, cognitive rehabilitation exercises, medication optimization, and addressing underlying sleep or medical issues.
What lifestyle changes can help reduce brain fog caused by depression?
Effective lifestyle changes include optimizing sleep quality and consistency, engaging in regular aerobic exercise, maintaining a balanced diet rich in omega-3s and antioxidants, practicing stress management techniques like meditation or yoga, staying socially connected, limiting alcohol and processed foods, and maintaining stable blood sugar levels. These modifications support overall brain health and cognitive function.
How long can brain fog last after depressive episodes or during remission?
Brain fog duration varies significantly among individuals. With effective depression treatment, cognitive improvements often begin within 4-8 weeks, though complete resolution may take several months. Some people experience lingering cognitive symptoms even after mood improvements, requiring targeted interventions. During remission, cognitive function typically continues improving gradually, but maintaining treatment and healthy habits is essential for preventing recurrence.