Diabetic neuropathy can significantly impact bladder function, leading to a range of uncomfortable and potentially serious urinary symptoms. When diabetes affects the nerves controlling the bladder, it can result in a condition known as neurogenic bladder, causing various complications in urinary function and control.
Understanding these bladder-related complications is crucial for diabetes patients and their healthcare providers to ensure proper management and prevent potential complications. This comprehensive guide explores the connection between diabetic neuropathy and bladder symptoms, along with effective treatment approaches and prevention strategies.
How Diabetes Affects Bladder Function
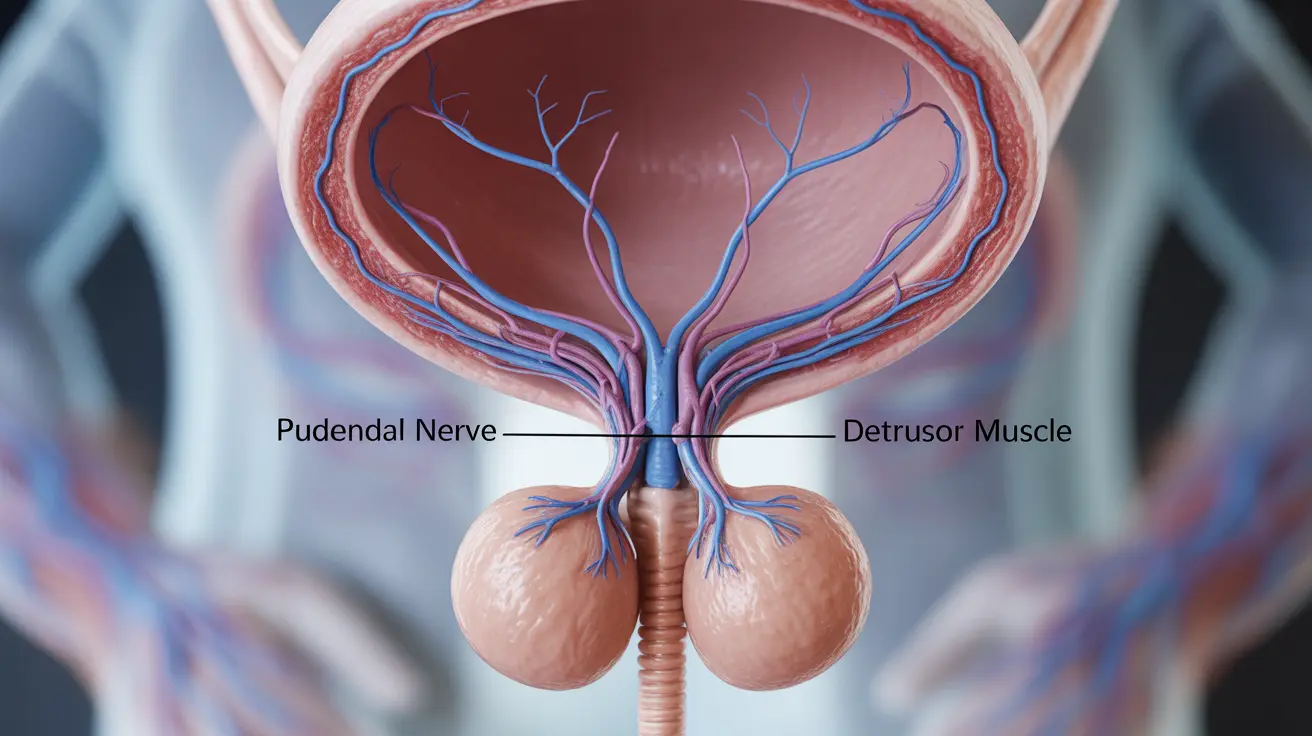
Diabetes can damage the nerves that control bladder function through prolonged exposure to high blood sugar levels. This nerve damage can affect both the sensation of needing to urinate and the muscles that control urination, leading to various bladder control problems.
The autonomic nervous system, which controls involuntary bodily functions including bladder control, is particularly vulnerable to diabetic neuropathy. When these nerves are damaged, they may not properly signal when the bladder is full or may not coordinate properly with the muscles that control urination.
Common Bladder Symptoms of Diabetic Neuropathy
Urinary Retention
One of the primary symptoms of diabetic neuropathy affecting the bladder is urinary retention. Patients may have difficulty completely emptying their bladder, leading to:
- Frequent urination
- Weak urine stream
- Difficulty starting urination
- Feeling of incomplete bladder emptying
Overactive Bladder
Diabetic neuropathy can also cause an overactive bladder, characterized by:
- Sudden, urgent needs to urinate
- Increased frequency of urination
- Nocturia (frequent nighttime urination)
- Occasional urinary incontinence
Diagnosis and Assessment
Healthcare providers typically use several methods to diagnose bladder problems related to diabetic neuropathy:
- Urodynamic testing
- Post-void residual measurement
- Bladder ultrasound
- Comprehensive neurological examination
- Urinalysis to check for infections
Treatment Options and Management
Medical Interventions
Several treatment approaches can help manage diabetic neuropathy bladder symptoms:
- Medications to improve bladder control
- Antimuscarinic drugs for overactive bladder
- Alpha-blockers for urinary retention
- Antibiotics when necessary for infections
Lifestyle Modifications
Implementing certain lifestyle changes can help manage symptoms:
- Scheduled voiding techniques
- Pelvic floor exercises
- Proper fluid management
- Bladder training exercises
Prevention and Blood Sugar Control
Maintaining good blood sugar control is essential in preventing or slowing the progression of diabetic neuropathy and its effects on bladder function. Regular monitoring of blood glucose levels and following prescribed diabetes management plans can help reduce the risk of developing bladder complications.
Frequently Asked Questions
What are the common bladder symptoms caused by diabetic neuropathy? Common symptoms include frequent urination, difficulty emptying the bladder completely, urgent need to urinate, and potential urinary incontinence. Some patients may also experience reduced bladder sensation.
How does diabetic neuropathy lead to urinary retention and infections? Diabetic neuropathy damages the nerves controlling bladder function, leading to incomplete bladder emptying. This retention can create an environment where bacteria can grow, increasing the risk of urinary tract infections.
What treatments are available for bladder problems caused by diabetic neuropathy? Treatment options include medications for bladder control, catheterization when necessary, lifestyle modifications, and pelvic floor exercises. Some patients may benefit from specialized devices or surgical interventions in severe cases.
Can controlling blood sugar levels help prevent diabetic neuropathy bladder symptoms? Yes, maintaining good blood sugar control is crucial in preventing or slowing the progression of diabetic neuropathy and its related bladder symptoms. Consistent blood sugar management can help protect nerve function.
How is neurogenic bladder from diabetes diagnosed and managed? Diagnosis typically involves urodynamic testing, physical examination, and various bladder function tests. Management includes a combination of medications, lifestyle modifications, and regular monitoring of bladder function and diabetes control.