When it comes to kidney health, understanding the distinction between kidney disease and kidney failure is crucial for proper diagnosis and treatment. These terms, while related, represent different stages and conditions affecting kidney function. This comprehensive guide will help you understand the key differences, their causes, symptoms, and treatment approaches.
What Defines Kidney Disease and Kidney Failure
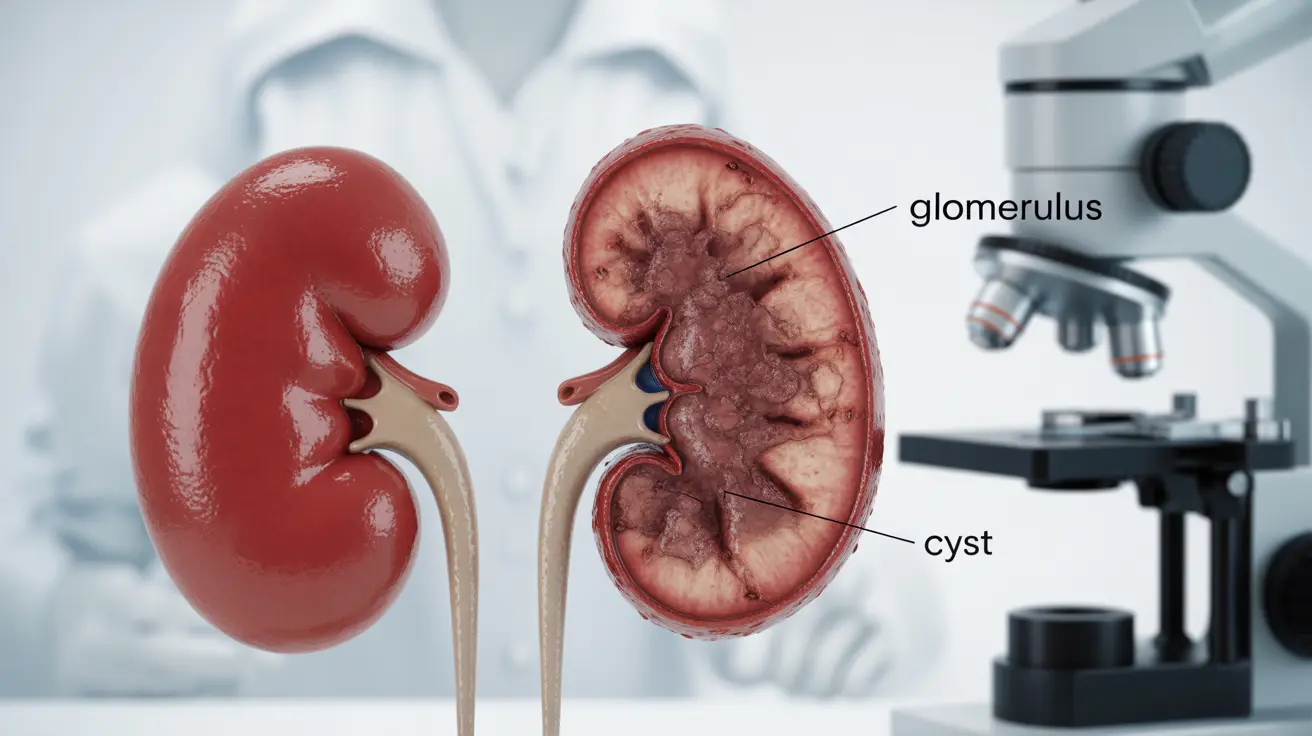
Kidney disease refers to any condition that damages your kidneys and affects their ability to filter waste from your blood. Kidney failure, on the other hand, occurs when your kidneys lose most or all of their function, requiring immediate medical intervention or dialysis to sustain life.
Acute vs. Chronic Conditions
Acute Kidney Injury (AKI)
Acute kidney injury, formerly known as acute renal failure, develops rapidly - usually within a few days or weeks. This sudden decline in kidney function is often reversible if identified and treated promptly.
Common causes of AKI include:
- Severe dehydration
- Major blood loss
- Severe infections
- Certain medications
- Urinary tract blockages
Chronic Kidney Disease (CKD)
Chronic kidney disease develops gradually over months or years, causing progressive and usually permanent damage to the kidneys. CKD typically progresses through five stages, with kidney failure being the final stage.
Common causes of CKD include:
- Diabetes
- High blood pressure
- Autoimmune diseases
- Genetic disorders
- Recurring kidney infections
Recognizing the Symptoms
Acute Kidney Injury Symptoms
AKI symptoms typically appear suddenly and may include:
- Decreased urine output
- Fluid retention and swelling
- Shortness of breath
- Confusion
- Chest pain or pressure
- Nausea and vomiting
Chronic Kidney Disease Symptoms
CKD symptoms develop gradually and may include:
- Fatigue and weakness
- Sleep problems
- Changes in urination
- Persistent itching
- Loss of appetite
- High blood pressure
- Anemia
Treatment Approaches
Managing Acute Kidney Injury
Treatment for AKI focuses on addressing the underlying cause and supporting kidney function until recovery. This may include:
- Temporary dialysis
- Medication adjustments
- Fluid management
- Treatment of infections
- Removal of urinary blockages
Managing Chronic Kidney Disease
CKD treatment aims to slow progression and manage complications through:
- Blood pressure control
- Dietary modifications
- Regular monitoring
- Medication management
- Lifestyle changes
- Eventual kidney replacement therapy (dialysis or transplant) if progression reaches end-stage
Frequently Asked Questions
What is the main difference between kidney disease and kidney failure? Kidney disease refers to any condition affecting kidney function, while kidney failure represents complete or near-complete loss of kidney function. Disease can progress to failure but doesn't always do so, especially with proper treatment.
How can acute kidney injury (acute renal failure) be distinguished from chronic kidney disease? Acute kidney injury develops rapidly over days or weeks and is potentially reversible, while chronic kidney disease develops slowly over months or years and typically causes permanent damage.
What are the common causes that lead to sudden kidney failure versus chronic kidney damage? Sudden kidney failure often results from severe dehydration, blood loss, infections, or medication reactions. Chronic kidney damage typically stems from ongoing conditions like diabetes, high blood pressure, or genetic disorders.
What symptoms should make me suspect acute kidney injury versus chronic kidney disease? Acute kidney injury presents with sudden symptoms like decreased urination, severe swelling, and confusion. Chronic kidney disease shows gradual symptoms like persistent fatigue, itching, and slow changes in urination patterns.
How are treatment approaches different for acute kidney injury compared to chronic kidney disease and kidney failure? Acute kidney injury treatment focuses on immediate intervention and reversing the cause, while chronic kidney disease treatment aims at slowing progression and managing complications long-term. End-stage kidney failure requires ongoing dialysis or transplantation.