Menopause brings significant changes to a woman's body, and digestive issues are among the most common yet least discussed symptoms. Understanding how to manage these digestive problems during menopause is crucial for maintaining quality of life and overall well-being. This comprehensive guide explores effective solutions and lifestyle modifications that can help alleviate digestive discomfort during this transitional period.
Understanding the Menopause-Digestion Connection
The hormonal fluctuations during menopause, particularly the decrease in estrogen levels, can significantly impact your digestive system. These changes can affect everything from how quickly food moves through your digestive tract to how efficiently your body processes nutrients. Understanding this connection is the first step in managing these symptoms effectively.
Common Digestive Symptoms During Menopause
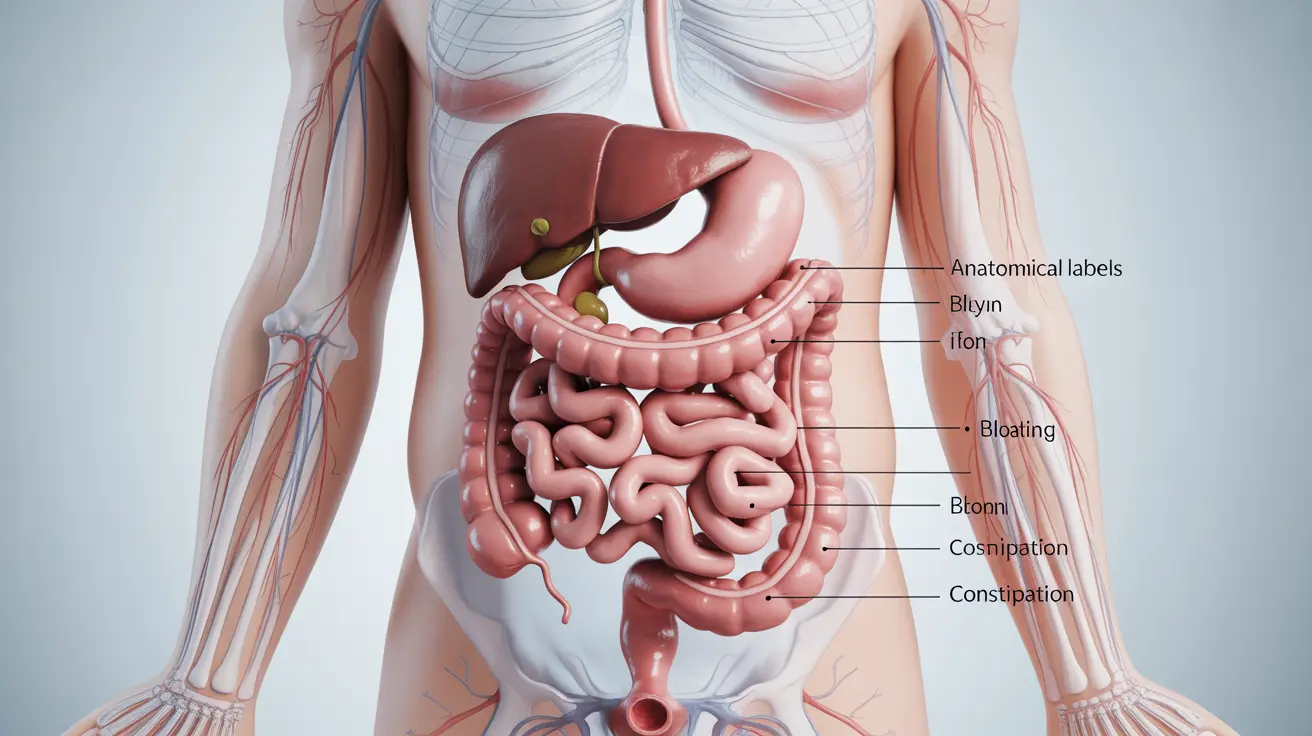
During menopause, women may experience various digestive issues, including:
- Bloating and gas
- Constipation
- Acid reflux
- Changes in appetite
- Irregular bowel movements
- Abdominal discomfort
Natural Solutions for Digestive Relief
Dietary Modifications
Making strategic changes to your diet can significantly improve digestive health during menopause:
- Include fiber-rich foods gradually
- Stay well-hydrated with water
- Incorporate lean proteins
- Choose whole grains over refined carbohydrates
- Add fermented foods to your diet
Lifestyle Changes
Implementing certain lifestyle modifications can help manage digestive problems effectively:
- Regular physical activity
- Stress management techniques
- Maintaining a consistent eating schedule
- Getting adequate sleep
- Avoiding trigger foods
The Role of Supplements and Probiotics
Certain supplements can support digestive health during menopause:
- Probiotics for gut health
- Digestive enzymes
- Magnesium supplements
- Vitamin D
- Calcium supplements
When to Seek Medical Help
While many digestive issues during menopause can be managed with lifestyle changes, certain symptoms warrant medical attention:
- Severe or persistent abdominal pain
- Unexplained weight loss
- Blood in stool
- Chronic diarrhea or constipation
- Frequent acid reflux
Frequently Asked Questions
What helps with digestive problems during menopause, and are there natural or lifestyle changes that can reduce symptoms like bloating and constipation?
Natural remedies include increasing fiber intake gradually, staying hydrated, regular exercise, and stress management techniques. Eating smaller, more frequent meals and avoiding trigger foods can also help reduce bloating and constipation.
How do hormonal changes during menopause affect digestion and what symptoms should I watch for?
Declining estrogen levels can slow digestive motility and affect gut bacteria balance. Watch for symptoms like bloating, constipation, acid reflux, and changes in bowel habits. These changes can also impact nutrient absorption and metabolism.
Can probiotics or specific foods improve gut health and reduce digestive discomfort during menopause?
Yes, probiotics can help maintain healthy gut flora and reduce digestive discomfort. Fermented foods, yogurt, fiber-rich vegetables, and whole grains can support digestive health during menopause.
Why do digestive issues sometimes get worse during menopause, and is there a link to stress or previous IBS?
Hormonal changes can exacerbate existing digestive conditions like IBS. Stress during menopause can further impact gut health through the gut-brain axis. Previous digestive issues may become more pronounced during this transitional period.
When should I see a doctor about digestive symptoms during menopause, and are there treatments or tests I should ask about?
Consult a healthcare provider if you experience severe or persistent symptoms, unexplained weight loss, or blood in stool. Your doctor may recommend tests to rule out other conditions and can discuss treatment options, including hormone therapy or specific medications for digestive issues.