Diverticulitis surgery represents a significant treatment option for individuals with severe or recurring diverticular disease. When conservative treatments like antibiotics and dietary changes prove insufficient, surgical intervention may become necessary to address complications and improve quality of life. Understanding the different surgical approaches, recovery expectations, and post-operative care is crucial for patients facing this procedure.
This comprehensive guide explores the various aspects of diverticulitis surgery, from determining when it's needed to managing recovery and potential complications. Whether you're considering surgery or preparing for an upcoming procedure, this information will help you make informed decisions about your care.
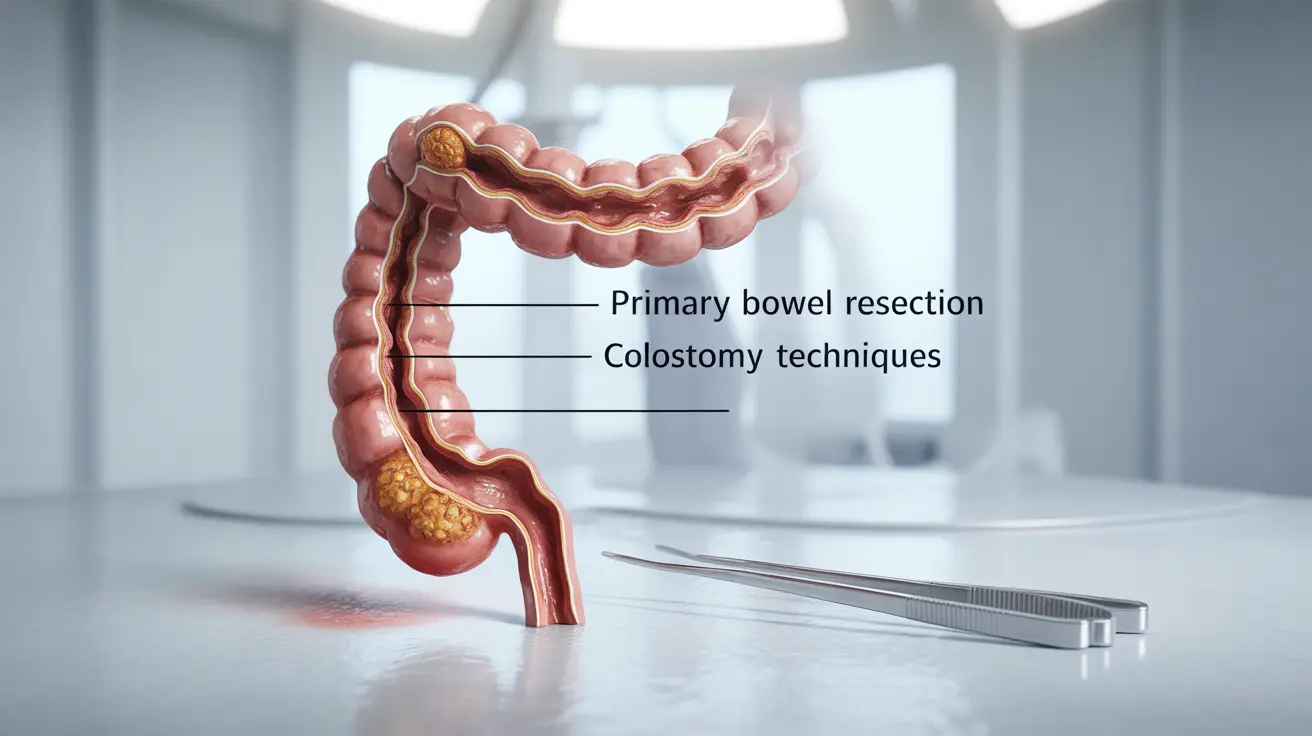
Types of Diverticulitis Surgery
There are several surgical approaches available for treating diverticulitis, each suited to different situations and patient needs:
Primary Bowel Resection (Sigmoidectomy)
This common procedure involves removing the diseased portion of the colon and reconnecting the healthy segments. It can be performed through traditional open surgery or using minimally invasive laparoscopic techniques, depending on the patient's condition and surgical requirements.
Bowel Resection with Colostomy
In more complex cases, particularly during emergency surgery or when inflammation is severe, a temporary or permanent colostomy may be necessary. This procedure involves creating an opening in the abdomen (stoma) to allow waste to exit into a collection bag.
When Surgery Becomes Necessary
Several factors may indicate the need for surgical intervention:
- Multiple episodes of acute diverticulitis
- Complications such as bowel obstruction or perforation
- Formation of fistulas
- Failure of conservative treatment approaches
- Chronic symptoms affecting quality of life
Preparing for Surgery
Proper preparation can significantly impact surgical outcomes. Key steps include:
- Complete medical evaluation
- Dietary modifications before surgery
- Bowel preparation procedures
- Discussion of medication adjustments
- Planning for post-operative care and support
Recovery Process and Timeline
Recovery from diverticulitis surgery varies depending on the surgical approach and individual factors. Most patients can expect:
Hospital Stay
Hospital stays typically range from 2-7 days, with longer periods possible for complex procedures or complications. During this time, medical staff monitor vital signs, manage pain, and guide early mobility efforts.
Post-Discharge Recovery
Complete recovery may take 4-6 weeks for laparoscopic surgery and 6-8 weeks for open surgery. Patients should follow specific guidelines for:
- Activity restrictions
- Dietary progression
- Wound care
- Follow-up appointments
Managing Complications and Risks
While generally safe, diverticulitis surgery carries potential risks including:
- Infection at the surgical site
- Bleeding
- Anastomotic leak
- Bowel obstruction
- Temporary bowel function changes
- Potential need for colostomy
Post-Surgery Diet and Nutrition
Proper nutrition plays a crucial role in recovery. Dietary recommendations typically progress through several stages:
- Clear liquids
- Full liquids
- Soft foods
- Regular diet with fiber modification
Frequently Asked Questions
What are the different types of diverticulitis surgery and how do they affect recovery?
The main types are primary bowel resection and bowel resection with colostomy. Laparoscopic procedures typically offer faster recovery times (4-6 weeks) compared to open surgery (6-8 weeks), with less post-operative pain and smaller incisions.
When is surgery recommended for diverticulitis instead of antibiotics or conservative treatments?
Surgery is recommended for recurring episodes, complications like perforation or fistulas, or when conservative treatments fail to provide relief. Emergency surgery may be necessary for severe complications like peritonitis.
What should I expect during the recovery period after diverticulitis surgery, including hospital stay and activity restrictions?
Expect a hospital stay of 2-7 days, followed by several weeks of restricted activities. Initial limitations include no heavy lifting and gradual return to normal activities, with full recovery typically taking 4-8 weeks depending on surgical approach.
What are the potential risks and complications associated with diverticulitis surgery?
Common risks include infection, bleeding, anastomotic leak, bowel obstruction, and changes in bowel function. Some patients may require temporary or permanent colostomy, particularly in emergency situations.
How do I manage diet and stoma care after diverticulitis surgery with colostomy?
Diet management involves a gradual progression from clear liquids to regular food, while stoma care requires regular cleaning, bag changes, and monitoring for complications. Working with a stoma nurse helps ensure proper care techniques and adjustment to life with a colostomy.