Seizures are intense neurological events that can raise concerns about potential damage to the brain. Understanding the relationship between seizures and brain damage is crucial for both patients and healthcare providers, as it helps inform treatment strategies and preventive measures.
While not all seizures cause permanent brain damage, certain types and circumstances can pose significant risks to brain health. This comprehensive guide explores the connection between seizures and brain injury, focusing on risk factors, prevention, and long-term implications.
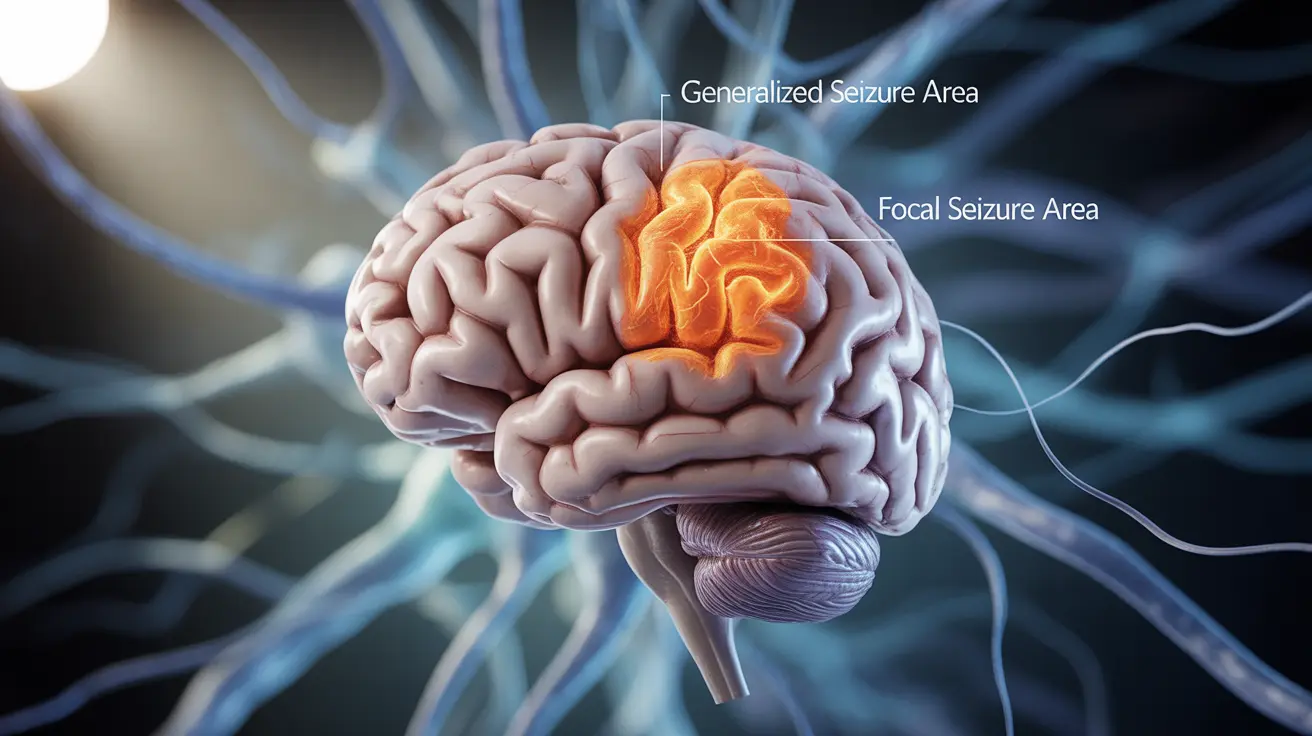
Types of Seizures and Their Impact on Brain Health
Different types of seizures carry varying levels of risk for brain damage. Generalized tonic-clonic seizures, which affect both sides of the brain simultaneously, typically pose a higher risk compared to focal seizures that impact only one area of the brain.
Status epilepticus, a condition where seizures last longer than 5 minutes or occur in clusters without recovery between episodes, presents the highest risk for permanent brain damage due to prolonged neural stress and oxygen deprivation.
Duration and Frequency: Critical Factors in Brain Injury Risk
The duration of seizures plays a crucial role in determining the potential for brain damage. Brief, isolated seizures rarely cause permanent harm to the brain. However, prolonged seizures can lead to:
- Neuronal death due to excessive electrical activity
- Oxygen deprivation in brain tissue
- Inflammation and structural changes in affected areas
- Metabolic disturbances affecting brain function
Frequent seizures may have cumulative effects on brain health, potentially leading to cognitive difficulties and memory problems over time.
Understanding Status Epilepticus and Its Consequences
Status epilepticus represents a medical emergency that requires immediate intervention. This condition can result in severe complications, including:
- Permanent cognitive impairment
- Changes in brain structure
- Increased risk of future seizures
- Development of drug-resistant epilepsy
Prevention and Management Strategies
Effective seizure control is essential for preventing brain damage. Key management approaches include:
- Consistent use of prescribed anti-epileptic medications
- Regular monitoring of seizure patterns
- Prompt medical attention for prolonged seizures
- Lifestyle modifications to reduce seizure triggers
- Regular consultations with healthcare providers
Special Considerations for Children
Children's developing brains may be particularly vulnerable to seizure-related damage. Febrile status epilepticus in young children requires special attention due to:
- Higher susceptibility to neurological complications
- Potential impact on cognitive development
- Increased risk of developing epilepsy later in life
- Need for careful monitoring and prompt intervention
Frequently Asked Questions
Can seizures cause permanent brain damage, and which types are most dangerous?
Yes, seizures can cause permanent brain damage, particularly in cases of status epilepticus or prolonged seizures lasting more than 5 minutes. Generalized tonic-clonic seizures and status epilepticus are typically the most dangerous types, especially when left untreated.
How does the duration and frequency of seizures affect the risk of brain injury?
Longer seizures and higher frequency significantly increase the risk of brain injury. Seizures lasting more than 5 minutes pose a greater risk of permanent damage, while frequent seizures can lead to cumulative effects on cognitive function and brain structure over time.
What are the long-term cognitive effects of prolonged seizures or status epilepticus?
Prolonged seizures and status epilepticus can result in memory problems, learning difficulties, attention deficits, and other cognitive impairments. These effects may be permanent and can impact daily functioning and quality of life.
How can effective seizure control reduce the risk of brain damage?
Effective seizure control through consistent medication use, lifestyle management, and prompt medical intervention for prolonged seizures significantly reduces the risk of brain damage. Regular monitoring and adherence to treatment plans are essential components of prevention.
Are children more vulnerable to brain damage from seizures, especially febrile status epilepticus?
Yes, children are generally more vulnerable to seizure-related brain damage due to their developing nervous systems. Febrile status epilepticus in children requires immediate medical attention as it can lead to more severe complications and long-term neurological effects.