Multiple sclerosis (MS) is a complex neurological condition that affects millions of people worldwide, and one of the most common questions patients and their families ask is whether the disease has a hereditary component. While MS is not directly inherited like some genetic disorders, research shows that family history does play a significant role in determining an individual's risk of developing this autoimmune condition.
Understanding the relationship between genetics and MS can help families make informed decisions about health monitoring and provide peace of mind about the actual level of risk involved. The connection between family history and MS involves a combination of genetic predisposition and environmental factors working together.
Understanding Multiple Sclerosis and Family Connections
Multiple sclerosis occurs when the immune system mistakenly attacks the protective covering of nerve fibers in the central nervous system. This autoimmune response leads to communication problems between the brain and the rest of the body, resulting in various neurological symptoms that can range from mild to severe.
Research has consistently shown that having a family member with MS does increase your risk of developing the condition, but it's important to understand that this increased risk is still relatively modest. The general population has approximately a 0.1% chance of developing MS, while individuals with a first-degree relative (parent, sibling, or child) with MS face a risk of about 2-5%.
This elevated risk suggests that genetic factors contribute to MS susceptibility, but the fact that the majority of people with affected family members never develop the condition indicates that genetics alone don't determine who will get MS.
Genetic Risk Factors in Multiple Sclerosis
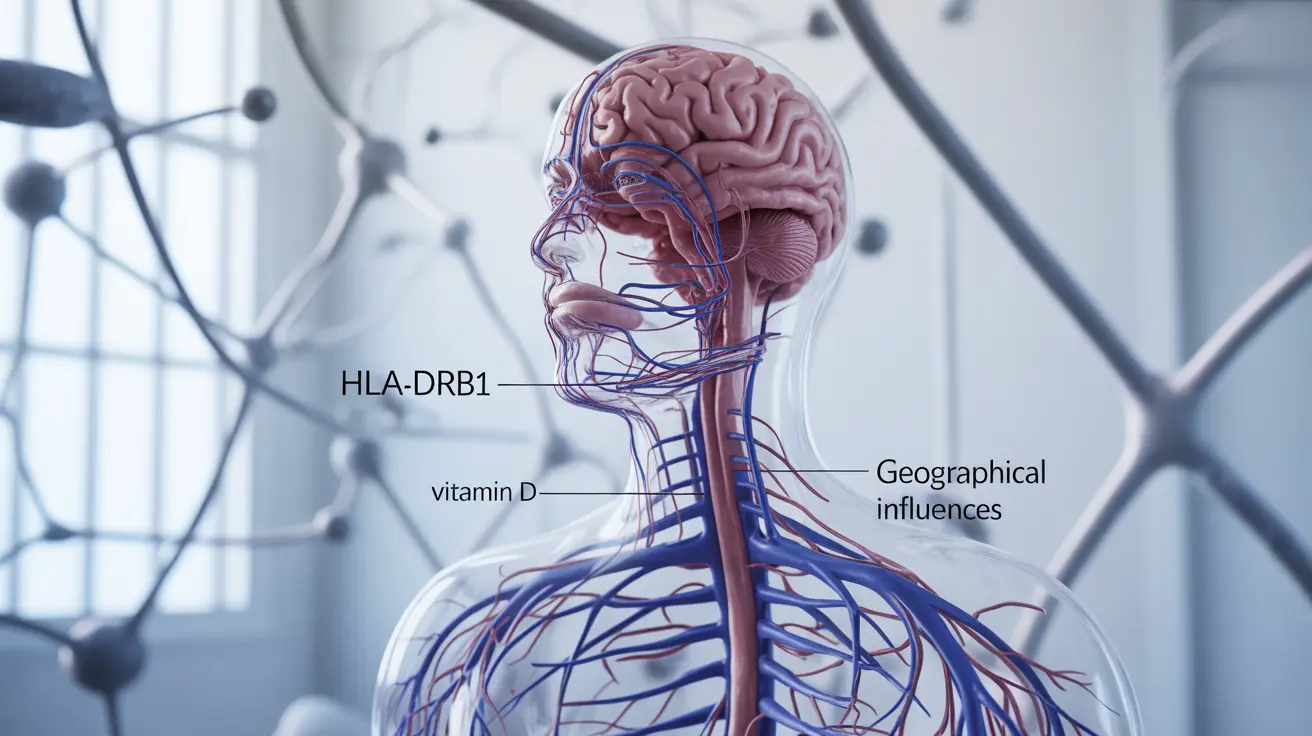
Scientists have identified more than 200 genetic variants that can influence MS risk, with the HLA-DRB1 gene being one of the most significant. This gene is part of the human leukocyte antigen system, which helps the immune system distinguish between the body's own cells and foreign substances.
Certain variations of HLA genes are found more frequently in people with MS, particularly those of Northern European ancestry. However, having these genetic markers doesn't guarantee that someone will develop MS – they simply increase susceptibility when combined with other risk factors.
Twin studies have provided valuable insights into the genetic component of MS. Identical twins, who share 100% of their DNA, have a concordance rate of about 25-30% for MS. This means that if one identical twin has MS, the other twin has roughly a 25-30% chance of also developing the condition. Fraternal twins, who share about 50% of their DNA like regular siblings, have a much lower concordance rate of around 3-5%.
Environmental Triggers and MS Development
While genetics provide the foundation for MS susceptibility, environmental factors often serve as the trigger that activates the disease process. These environmental influences help explain why not everyone with genetic risk factors develops MS and why the condition can appear in people with no family history.
Several environmental factors have been associated with increased MS risk, including vitamin D deficiency, certain viral infections (particularly Epstein-Barr virus), smoking, and geographic location. People living farther from the equator have higher rates of MS, possibly due to reduced sun exposure and lower vitamin D levels.
The interaction between genetic predisposition and environmental triggers follows what researchers call the "multiple hit" hypothesis. This theory suggests that multiple factors must align – including genetic susceptibility, environmental exposures, and possibly other unknown elements – for MS to develop.
MS Risk in Different Family Relationships
The degree of genetic relationship affects the level of MS risk. First-degree relatives (parents, siblings, and children) of someone with MS have the highest increased risk, facing odds that are 20-40 times higher than the general population, though this still translates to only a 2-5% absolute risk.
Second-degree relatives, such as aunts, uncles, nieces, nephews, and grandparents, have a smaller but still elevated risk compared to the general population. Third-degree relatives and more distant family members show risk levels that approach those of the general population.
Interestingly, the risk appears to be slightly higher when the affected family member is female, which may relate to the fact that women are two to three times more likely to develop MS than men.
When MS Occurs Without Family History
It's crucial to understand that the vast majority of people with MS – approximately 85-90% – have no known family history of the condition. This statistic demonstrates that while family history increases risk, it's far from necessary for MS development.
Several factors explain why MS can occur in people without affected relatives. First, the condition may have occurred in previous generations but went undiagnosed, as MS recognition and diagnostic capabilities have improved significantly over the past several decades. Second, the genetic risk factors may be present but never activated due to the absence of appropriate environmental triggers in previous generations.
Additionally, new genetic mutations can occur, and the complex interplay of multiple genes means that risk factors can combine in ways that weren't present in previous family members.
Implications for Families and Genetic Counseling
For families affected by MS, understanding the genetic component can be both reassuring and concerning. While there is an increased risk for family members, the absolute risk remains relatively low, and many factors beyond genetics influence whether someone will develop the condition.
Genetic counseling can be valuable for families dealing with MS, particularly when planning for children or when multiple family members are affected. Counselors can help families understand their specific risk factors, discuss the latest research, and provide guidance on monitoring and prevention strategies.
Currently, there are no genetic tests that can definitively predict who will develop MS, as the condition involves too many variables and genetic factors. However, research in this area continues to advance, and future developments may provide more precise risk assessment tools.
Frequently Asked Questions
Does multiple sclerosis run in families?
Yes, multiple sclerosis does show a familial tendency, meaning it occurs more frequently in some families than would be expected by chance. However, MS is not directly inherited like single-gene disorders. Instead, family members share genetic susceptibility factors that can increase the likelihood of developing MS when combined with environmental triggers. The risk is elevated but still relatively modest for most family members.
What is the risk of getting MS if a parent or sibling has it?
If you have a parent or sibling with MS, your risk of developing the condition is approximately 2-5%, compared to the general population risk of about 0.1%. While this represents a 20-40 fold increase in relative risk, the absolute risk remains quite low, meaning that 95-98% of people with an affected first-degree relative will never develop MS themselves.
Is multiple sclerosis inherited or genetic?
Multiple sclerosis has a genetic component but is not directly inherited in a predictable pattern like some genetic diseases. Instead, MS involves complex genetic susceptibility involving more than 200 genetic variants that can influence risk. These genetic factors increase susceptibility to MS, but environmental triggers are typically needed to activate the disease process. This explains why identical twins have only a 25-30% concordance rate for MS despite sharing identical DNA.
Can you get MS if no one in your family has it?
Absolutely. About 85-90% of people with MS have no known family history of the condition. MS can develop due to the complex interaction of genetic susceptibility factors and environmental triggers, and these genetic factors may not have been activated in previous generations, or the condition may have gone undiagnosed in earlier family members when diagnostic capabilities were more limited.
What are the main genetic and environmental risk factors for multiple sclerosis?
The main genetic risk factors include variations in the HLA-DRB1 gene and more than 200 other genetic variants that influence immune system function. Key environmental risk factors include vitamin D deficiency, Epstein-Barr virus infection, smoking, geographic location (higher rates farther from the equator), and possibly other viral infections. The interaction between genetic predisposition and environmental triggers determines who ultimately develops MS, following what researchers call the "multiple hit" hypothesis.