Fetal alcohol syndrome (FAS) represents one of the most preventable causes of birth defects and developmental disabilities in children. For expectant mothers and those planning pregnancy, understanding the relationship between alcohol consumption and fetal development is crucial for making informed decisions about their health and their baby's wellbeing.
The question of how much drinking causes fetal alcohol syndrome doesn't have a simple answer, as multiple factors influence the risk. However, medical experts universally agree that no amount of alcohol has been proven safe during pregnancy, making complete abstinence the only guaranteed way to prevent alcohol-related birth defects.
Understanding Fetal Alcohol Syndrome
Fetal alcohol syndrome is a severe form of fetal alcohol spectrum disorder (FASD) that occurs when alcohol crosses the placenta and interferes with the developing baby's growth and organ development. Unlike many other birth defects, FAS is entirely preventable through maternal alcohol abstinence during pregnancy.
The condition affects multiple aspects of a child's development, including physical growth, facial features, central nervous system function, and cognitive abilities. Children with FAS may experience lifelong challenges including learning disabilities, behavioral problems, and difficulties with social interaction.
The Dose-Response Relationship: No Safe Threshold
Research consistently shows that there is no established safe threshold for alcohol consumption during pregnancy. Even small amounts of alcohol can potentially harm the developing fetus, particularly during critical periods of organ development in the first trimester.
Studies have demonstrated that the risk of fetal alcohol syndrome increases with both the amount and frequency of alcohol consumption. However, individual cases have been documented where relatively small amounts of alcohol resulted in significant fetal damage, while some heavy drinkers gave birth to apparently unaffected children.
This variability doesn't diminish the importance of abstinence, as it's impossible to predict which pregnancies will be most vulnerable to alcohol's effects. The developing brain is particularly susceptible to alcohol throughout the entire pregnancy, not just during the first trimester.
Binge Drinking: Heightened Risks for Fetal Development
Binge drinking during pregnancy poses especially severe risks for fetal development. Defined as consuming four or more drinks in a single occasion, binge drinking creates high blood alcohol concentrations that can be particularly damaging to the developing fetus.
During binge drinking episodes, the fetus is exposed to toxic levels of alcohol for extended periods. This pattern of consumption is associated with more severe forms of fetal alcohol spectrum disorders, including the full syndrome. The rapid consumption overwhelms the body's ability to metabolize alcohol efficiently, leading to prolonged exposure of the developing baby to high alcohol concentrations.
Even a single binge drinking episode during pregnancy can potentially cause permanent damage, particularly if it occurs during critical developmental windows when organs and systems are forming.
Timing Matters: Early Pregnancy Vulnerability
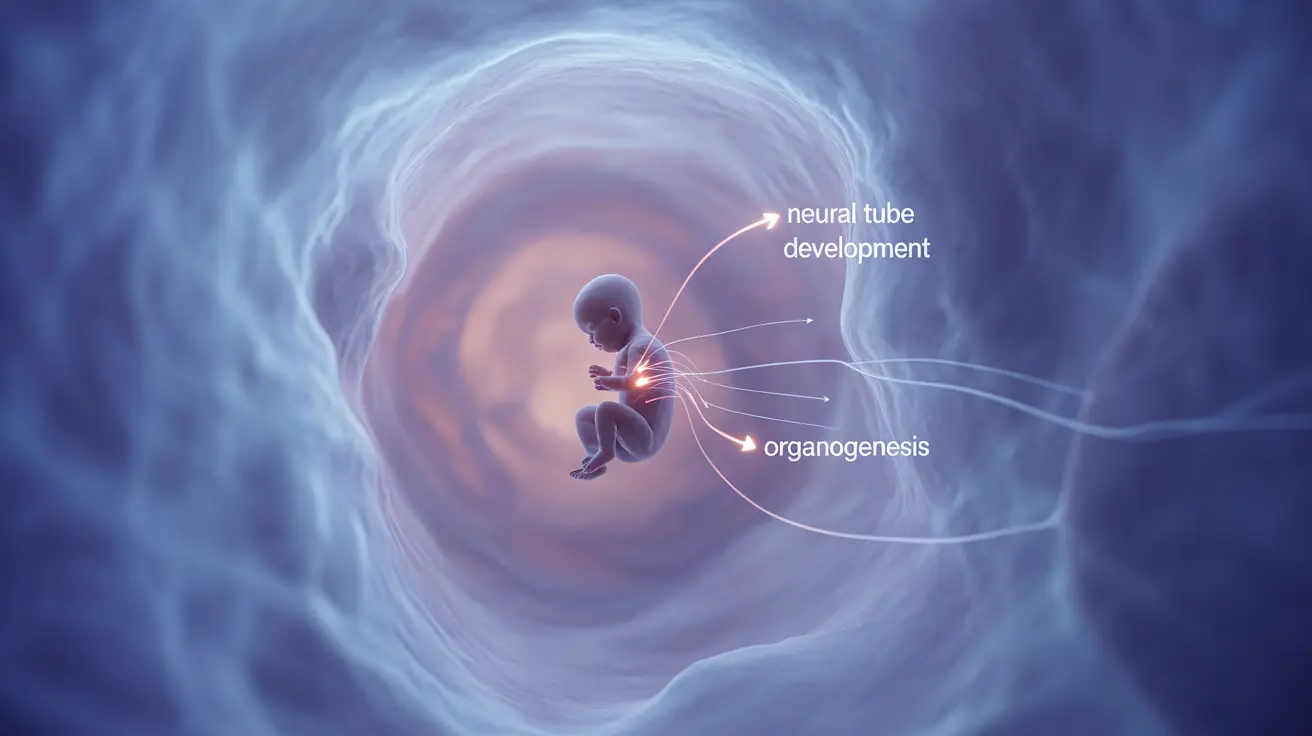
The timing of alcohol exposure during pregnancy significantly influences the type and severity of potential damage. Early pregnancy, particularly the first trimester, represents a critical period when major organ systems are developing.
During the first few weeks after conception, many women don't yet know they're pregnant. Alcohol consumption during this period can interfere with neural tube formation, brain development, and the formation of facial features characteristic of fetal alcohol syndrome.
However, it's important to understand that the brain continues developing throughout pregnancy, meaning alcohol can cause damage at any point during gestation. The third trimester is particularly crucial for brain growth and development, making abstinence important throughout the entire pregnancy.
Factors Influencing Risk Beyond Alcohol Amount
While the amount of alcohol consumed is a primary factor in determining risk, several other variables can influence the likelihood and severity of fetal alcohol syndrome:
- Maternal metabolism plays a crucial role, as genetic variations in alcohol-metabolizing enzymes can affect how quickly alcohol is processed. Women who metabolize alcohol more slowly may subject their fetus to longer periods of exposure.
- Nutritional status significantly impacts risk, as poor nutrition, particularly deficiencies in folate, zinc, and other essential nutrients, can increase vulnerability to alcohol's effects. Malnutrition combined with alcohol consumption creates a particularly dangerous environment for fetal development.
- Pattern of drinking matters as much as total consumption. Regular daily drinking may be more harmful than occasional consumption of the same total amount, as it provides constant exposure without recovery periods.
- Maternal age and health status also influence risk. Older mothers may have decreased ability to metabolize alcohol, while underlying health conditions can compound alcohol's effects on fetal development.
Prevention and Support
The most effective prevention strategy for fetal alcohol syndrome is complete alcohol abstinence during pregnancy and while trying to conceive. For women who struggle with alcohol dependence, seeking professional help before and during pregnancy is crucial.
Healthcare providers can offer resources including counseling, support groups, and medical assistance for alcohol cessation. Many communities provide specialized programs for pregnant women dealing with substance use issues.
Partner and family support plays a vital role in successful alcohol abstinence during pregnancy. Creating an alcohol-free environment and understanding the importance of abstinence helps expectant mothers maintain their commitment to their baby's health.
Frequently Asked Questions
How much alcohol consumption during pregnancy causes fetal alcohol syndrome?
There is no established safe amount of alcohol consumption during pregnancy that guarantees prevention of fetal alcohol syndrome. Even small amounts can potentially cause harm, which is why medical experts recommend complete abstinence. The risk increases with both the quantity and frequency of alcohol consumption, but individual vulnerability varies significantly.
Is there a safe amount of alcohol a pregnant woman can drink without risking fetal alcohol syndrome?
No safe amount of alcohol during pregnancy has been established by medical research. While some studies suggest that very light, infrequent drinking may carry lower risks, no threshold has been identified below which harm is impossible. The only way to completely eliminate the risk of fetal alcohol syndrome is total abstinence from alcohol during pregnancy.
Why is binge drinking during pregnancy especially dangerous for fetal development?
Binge drinking creates extremely high blood alcohol levels that expose the fetus to toxic concentrations for extended periods. This pattern overwhelms the body's ability to process alcohol efficiently, leading to prolonged fetal exposure. Binge drinking is associated with more severe forms of fetal alcohol spectrum disorders and can cause significant damage even from a single episode, particularly during critical developmental periods.
Can drinking small amounts of alcohol early in pregnancy still harm the baby?
Yes, even small amounts of alcohol consumed early in pregnancy can potentially harm the developing baby. The first trimester is particularly critical as major organ systems and facial features are forming. During the earliest weeks, when many women don't yet know they're pregnant, alcohol can interfere with crucial developmental processes including neural tube formation and brain development.
What factors influence the risk of fetal alcohol syndrome besides the amount of alcohol consumed?
Several factors beyond alcohol quantity influence FAS risk, including maternal metabolism and genetic variations in alcohol-processing enzymes, nutritional status (particularly folate and zinc levels), drinking patterns (daily versus occasional), maternal age and overall health, timing of alcohol exposure during pregnancy, and environmental factors. Poor nutrition combined with alcohol consumption creates particularly high risk for fetal damage.