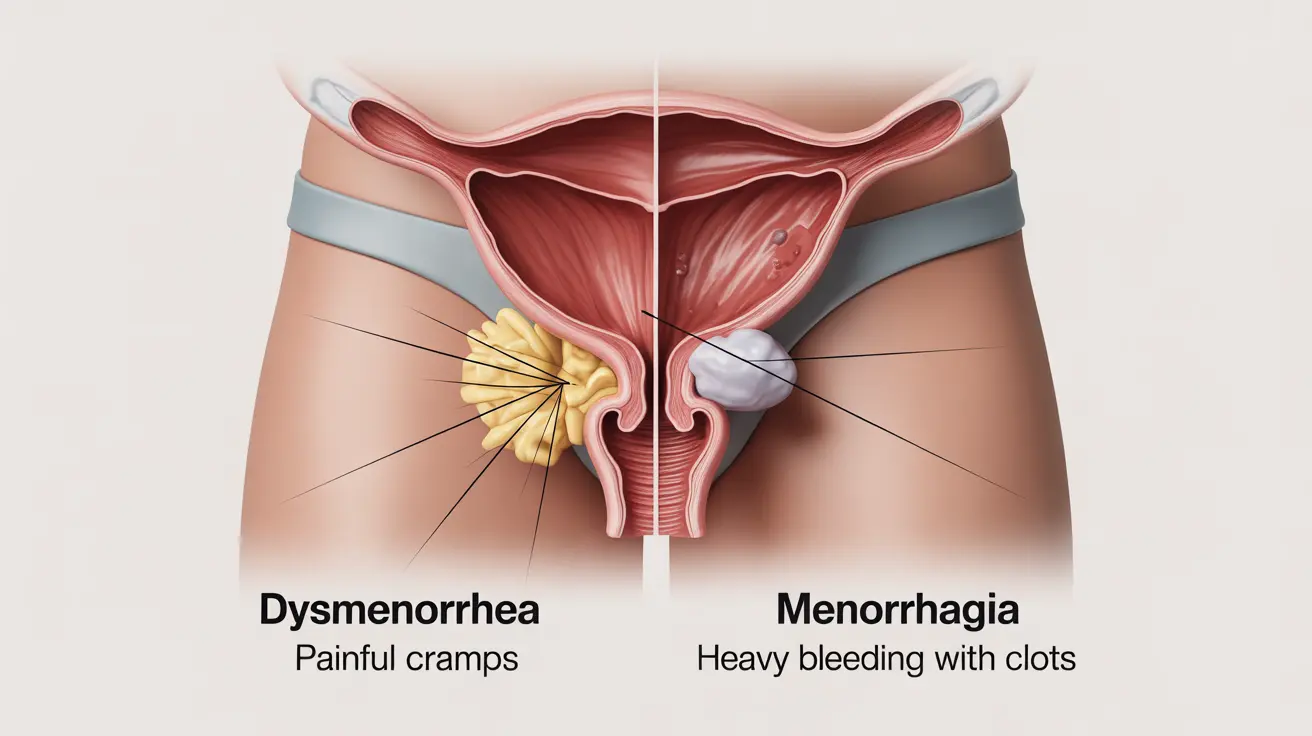
When it comes to menstrual health issues, understanding the distinction between dysmenorrhea and menorrhagia is crucial for proper diagnosis and treatment. While both conditions affect menstruation, they represent different types of menstrual disorders that require specific approaches to management.
This comprehensive guide explores the key differences between these two common menstrual conditions, helping you better understand their symptoms, causes, and treatment options.
Defining the Conditions
What is Dysmenorrhea?
Dysmenorrhea refers to painful menstrual cramps and discomfort during menstruation. This condition can be primary (occurring naturally) or secondary (caused by underlying conditions). The pain typically concentrates in the lower abdomen but may radiate to the lower back and thighs.
What is Menorrhagia?
Menorrhagia describes abnormally heavy or prolonged menstrual bleeding. Women with this condition experience excessive blood loss that can significantly interfere with daily activities and may lead to iron-deficiency anemia if left untreated.
Key Differences in Symptoms
Dysmenorrhea Symptoms
Common symptoms of dysmenorrhea include:
- Cramping pain in the lower abdomen
- Lower back pain
- Nausea and vomiting
- Headaches
- Fatigue
- Diarrhea or constipation
Menorrhagia Symptoms
Characteristic signs of menorrhagia include:
- Bleeding that lasts longer than 7 days
- Needing to change menstrual products every hour
- Passing large blood clots
- Bleeding through clothes or bedding
- Fatigue and shortness of breath due to anemia
Diagnosis Methods
Diagnosing Dysmenorrhea
Healthcare providers typically diagnose dysmenorrhea through:
- Detailed medical history
- Physical examination
- Pelvic exam
- Ultrasound (if secondary dysmenorrhea is suspected)
Diagnosing Menorrhagia
Menorrhagia diagnosis often involves:
- Blood tests to check for anemia
- Pelvic examination
- Ultrasound imaging
- Endometrial biopsy in some cases
- Hysteroscopy when necessary
Treatment Approaches
Managing Dysmenorrhea
Treatment options for dysmenorrhea typically include:
- Over-the-counter pain relievers
- Hormonal birth control
- Heat therapy
- Lifestyle modifications
- Treatment of underlying conditions (for secondary dysmenorrhea)
Managing Menorrhagia
Menorrhagia treatment may involve:
- Hormonal medications
- Tranexamic acid
- Iron supplements for anemia
- Surgical options in severe cases
- Treatment of underlying medical conditions
Frequently Asked Questions
What is the difference between dysmenorrhea and menorrhagia?
Dysmenorrhea primarily involves painful menstrual cramps and discomfort, while menorrhagia refers to abnormally heavy or prolonged menstrual bleeding. The main distinction lies in their primary symptoms: pain versus excessive bleeding.
What are the common symptoms of menorrhagia and how does it affect daily life?
Menorrhagia symptoms include heavy bleeding lasting more than 7 days, frequent changing of menstrual products, and passing large blood clots. It can significantly impact daily activities, cause fatigue, and lead to anemia if untreated.
How is menorrhagia diagnosed and what tests are usually done?
Menorrhagia diagnosis typically involves blood tests, pelvic examination, ultrasound imaging, and sometimes endometrial biopsy or hysteroscopy. Doctors will also review the patient's medical history and menstrual patterns.
What treatment options are available for managing heavy menstrual bleeding caused by menorrhagia?
Treatment options include hormonal medications, tranexamic acid, iron supplements, and surgical interventions in severe cases. The choice of treatment depends on the underlying cause and severity of symptoms.
Can NSAIDs used for dysmenorrhea increase bleeding in women with menorrhagia?
While NSAIDs are effective for managing dysmenorrhea pain, some women with menorrhagia should use them cautiously. It's important to consult with a healthcare provider, as certain NSAIDs may affect blood clotting and potentially impact menstrual flow.