Dealing with a persistent ear infection that refuses to respond to antibiotic treatment can be both frustrating and concerning. While antibiotics are typically the first line of defense against bacterial ear infections, there are instances where these medications may not provide the expected relief, leaving patients wondering about their next steps.
Understanding why ear infections sometimes resist antibiotic treatment and knowing what alternative options are available can help you make informed decisions about your healthcare. This comprehensive guide explores the reasons behind antibiotic-resistant ear infections and outlines effective strategies for managing persistent symptoms.
Understanding Antibiotic Resistance in Ear Infections
When an ear infection doesn't respond to antibiotics, several factors could be at play. The most common reason is that the infection may be viral rather than bacterial. Antibiotics are specifically designed to combat bacterial infections and have no effect on viruses, which means a viral ear infection will naturally run its course regardless of antibiotic treatment.
Another significant factor is bacterial resistance. Some strains of bacteria have developed resistance to commonly prescribed antibiotics, making standard treatments less effective. This resistance can occur when bacteria mutate or when antibiotics are used inappropriately, such as not completing a full course of medication or taking antibiotics for viral infections.
Additionally, the specific type of bacteria causing the infection may require a different antibiotic than what was initially prescribed. Laboratory cultures can help identify the exact bacterial strain and determine which antibiotics will be most effective against it.
Alternative Treatment Approaches for Persistent Ear Infections
When antibiotics fail to resolve an ear infection, healthcare providers have several alternative treatment options to consider. Pain management becomes a priority, and over-the-counter pain relievers such as ibuprofen or acetaminophen can provide significant relief while addressing inflammation.
Warm compresses applied to the affected ear can help reduce pain and promote drainage. Some patients find relief through ear drops containing numbing agents or anti-inflammatory medications, which can be particularly helpful for managing discomfort.
In cases where fluid buildup is a primary concern, decongestants may help improve drainage from the ear. However, these should only be used under medical supervision, as they can have side effects and may not be appropriate for all patients.
Natural and Supportive Remedies
Several natural approaches can complement medical treatment for persistent ear infections. Staying well-hydrated helps thin mucus and promotes better drainage, while humidifying the air can prevent the ear canal from becoming too dry.
Some patients benefit from gentle ear irrigation performed by a healthcare professional, which can help remove excess wax or debris that might be contributing to the infection. However, this procedure should never be attempted at home, as improper technique can cause further damage.
Recognizing Serious Complications
Untreated or poorly managed ear infections can lead to several serious complications that require immediate medical attention. One of the most concerning complications is mastoiditis, an infection of the bone behind the ear that can cause severe pain, swelling, and even hearing loss if not treated promptly.
Chronic ear infections can also result in permanent hearing damage, particularly in children whose hearing is still developing. The repeated inflammation and fluid buildup can damage the delicate structures within the ear, leading to conductive or even sensorineural hearing loss.
In rare cases, untreated ear infections can spread to nearby areas, potentially causing meningitis, brain abscesses, or facial nerve paralysis. These complications underscore the importance of seeking appropriate medical care when standard treatments fail.
When Surgery Becomes Necessary
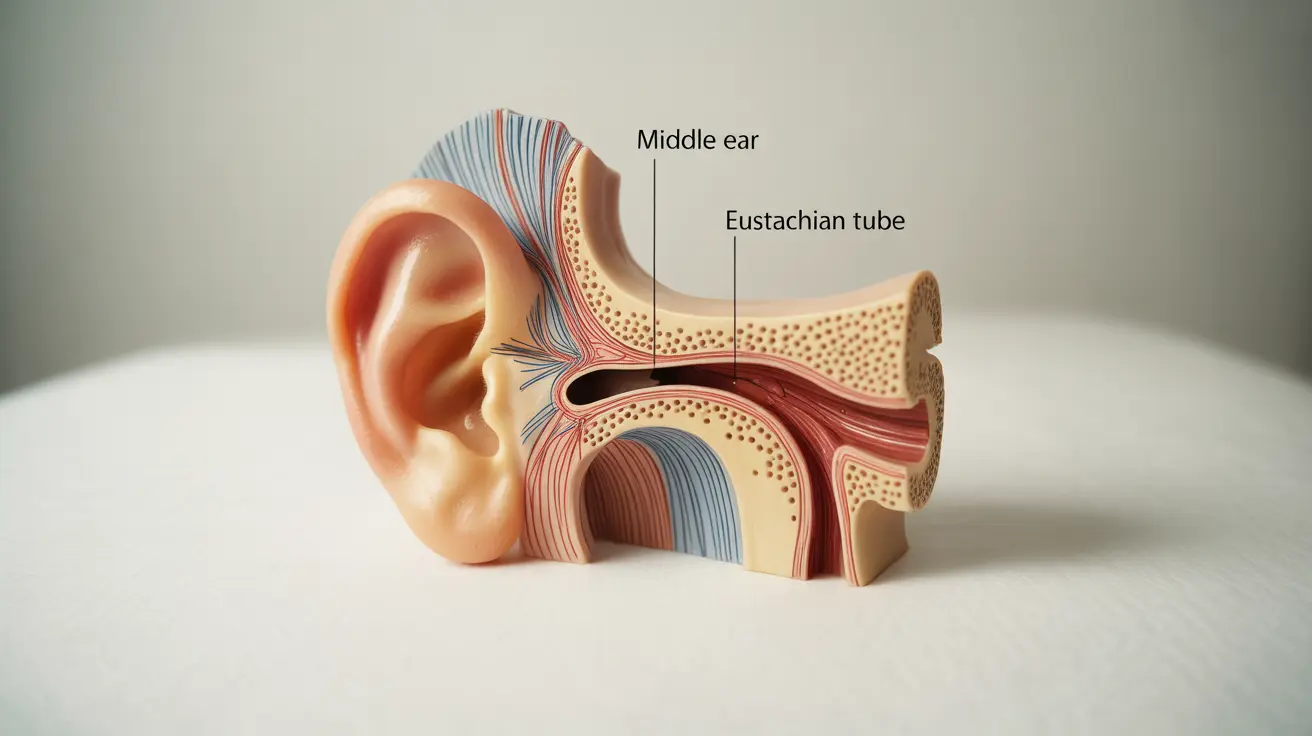
Surgical intervention may be recommended when conservative treatments have failed and complications are likely to develop. The most common surgical procedure for chronic ear infections is myringotomy with tube placement, where tiny tubes are inserted into the eardrum to promote drainage and prevent fluid buildup.
This outpatient procedure is particularly effective for children who experience recurrent ear infections or have persistent fluid behind the eardrum. The tubes typically remain in place for several months to a few years, during which time they help maintain proper ear ventilation.
In more severe cases, procedures such as mastoidectomy may be necessary to remove infected tissue from the mastoid bone. This surgery is typically reserved for cases where the infection has spread beyond the middle ear and poses a risk of serious complications.
Recovery and Follow-up Care
Post-surgical care is crucial for optimal outcomes. Patients must keep their ears dry during the healing process and follow all post-operative instructions carefully. Regular follow-up appointments allow healthcare providers to monitor healing progress and address any concerns that arise.
Most patients experience significant improvement in their symptoms following appropriate surgical intervention, with reduced frequency of ear infections and improved hearing function.
Frequently Asked Questions
What should I do if my ear infection does not go away after taking antibiotics?
If your ear infection persists after completing a full course of antibiotics, contact your healthcare provider immediately. They may need to perform additional tests, prescribe a different antibiotic, or explore alternative treatment options. Never attempt to self-treat with leftover antibiotics or over-the-counter remedies without medical guidance.
What are the possible reasons an ear infection doesn't respond to antibiotic treatment?
Several factors can cause antibiotic resistance in ear infections. The infection may be viral rather than bacterial, making antibiotics ineffective. Bacterial resistance, incomplete antibiotic courses, or the wrong type of antibiotic for the specific bacterial strain can also contribute to treatment failure. Additionally, anatomical issues or underlying conditions may prevent proper drainage and healing.
Are there other treatment options besides antibiotics for persistent or chronic ear infections?
Yes, several alternative treatments are available for persistent ear infections. These include pain management with over-the-counter medications, warm compresses, prescription ear drops, decongestants for drainage improvement, and professional ear cleaning. In some cases, addressing underlying conditions like allergies or sinus problems can help resolve chronic ear infections.
What are the long-term risks or complications if an ear infection is not treated successfully?
Untreated ear infections can lead to serious complications including permanent hearing loss, mastoiditis (infection of the bone behind the ear), chronic drainage, eardrum perforation, and in rare cases, meningitis or brain abscesses. Children are particularly vulnerable to hearing-related developmental issues if chronic ear infections are left untreated.
When is surgery needed for an ear infection that doesn't heal with medication, and what types of surgeries are available?
Surgery is typically considered when multiple antibiotic courses have failed, complications develop, or there's persistent fluid buildup affecting hearing. Common procedures include myringotomy with tube placement for drainage, tympanoplasty to repair the eardrum, and mastoidectomy to remove infected bone tissue. The specific procedure depends on the severity and location of the infection.