The relationship between fasting and cancer has become an increasingly important area of medical research, as scientists explore how dietary interventions might complement traditional cancer treatments. While cancer patients have long been advised to maintain adequate nutrition, emerging evidence suggests that strategic periods of fasting may offer unique benefits in certain contexts.
Understanding the complex interactions between fasting and cancer requires careful examination of both potential benefits and significant risks. This comprehensive approach is essential for patients and healthcare providers making informed decisions about incorporating fasting protocols into cancer care plans.
The Science Behind Fasting and Cancer Cell Biology
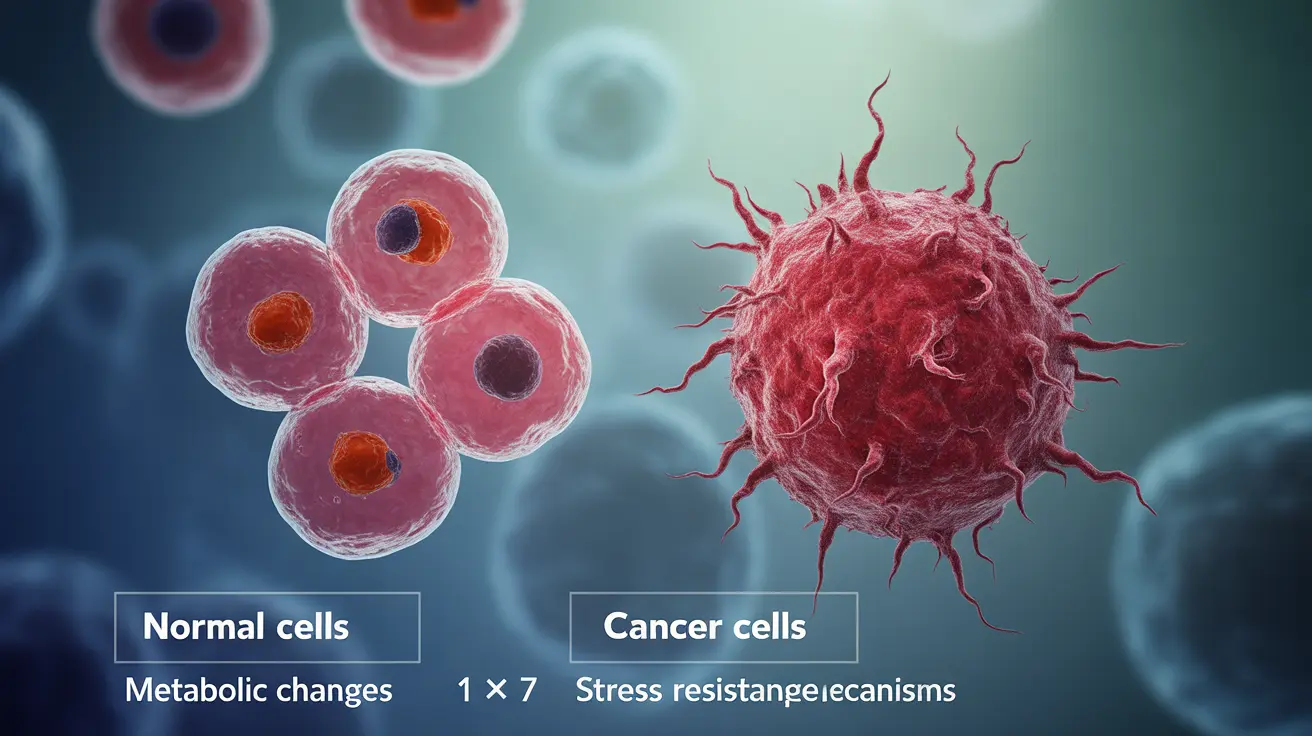
Research into fasting and cancer reveals fascinating mechanisms at the cellular level. During periods of food restriction, normal cells enter a protective state that helps them withstand stress, including the stress caused by chemotherapy drugs. This phenomenon, known as differential stress resistance, may create a therapeutic window where cancer cells become more vulnerable to treatment while healthy cells gain protection.
Studies indicate that fasting triggers metabolic changes that can influence cancer cell growth patterns. When the body enters a fasted state, glucose levels drop and ketone production increases. Cancer cells, which often rely heavily on glucose for energy, may struggle to adapt to this altered metabolic environment more than healthy cells.
The autophagy process, enhanced during fasting periods, plays a crucial role in cellular cleanup and may help remove damaged cellular components that could contribute to cancer development or progression. This natural cellular recycling mechanism becomes more active when nutrients are temporarily restricted.
Potential Benefits for Cancer Treatment Enhancement
Clinical trials have explored whether fasting can enhance the effectiveness of conventional cancer treatments. Some research suggests that short-term fasting before chemotherapy sessions may reduce treatment-related side effects while potentially improving therapeutic outcomes.
The concept of sensitizing cancer cells to treatment through metabolic manipulation shows promise in laboratory studies. Fasting may make certain types of cancer cells more susceptible to chemotherapy drugs, radiation therapy, or immunotherapy approaches.
Additionally, some studies indicate that fasting might help reduce treatment-related toxicity in healthy tissues. This protective effect could allow for more aggressive treatment protocols while minimizing damage to normal cells throughout the body.
Understanding the Risks and Safety Concerns
Cancer patients face unique nutritional challenges that make fasting particularly risky without proper medical supervision. Many individuals undergoing cancer treatment already struggle with maintaining adequate nutrition due to treatment side effects, reduced appetite, or metabolic changes associated with their disease.
Weight loss and muscle wasting are serious concerns for cancer patients, and inappropriate fasting could accelerate these dangerous processes. Malnutrition can weaken the immune system, slow healing, and reduce the body's ability to tolerate necessary treatments.
Certain cancer treatments may interact poorly with fasting states. Patients receiving specific medications or those with particular types of cancer may face increased risks when combining their treatment regimen with periods of food restriction.
The Role of Healthcare Provider Supervision
Any consideration of fasting during cancer treatment must involve close collaboration with oncologists, registered dietitians, and other healthcare team members. Professional guidance ensures that fasting protocols, if appropriate, are tailored to individual patient needs and medical circumstances.
Healthcare providers can assess whether a patient's current health status, treatment plan, and nutritional reserves make fasting a viable option. They can also monitor for potential complications and adjust approaches as treatment progresses.
Regular monitoring of blood markers, nutritional status, and treatment response becomes even more critical when fasting is incorporated into a cancer care plan. This oversight helps ensure that any dietary interventions support rather than compromise treatment goals.
Current Research and Future Directions
Ongoing clinical trials continue to investigate the safety and efficacy of various fasting approaches in cancer care. These studies examine different fasting durations, timing relative to treatments, and patient populations to better define when and how fasting might be beneficial.
Researchers are also exploring modified fasting approaches, such as fasting-mimicking diets, that may provide some benefits of complete fasting while reducing risks. These protocols typically involve severely restricted calorie intake rather than complete food avoidance.
The field continues to evolve as scientists work to identify which patients might benefit most from fasting interventions and how to implement these approaches safely within existing treatment frameworks.
Frequently Asked Questions
Can fasting help with cancer treatment and make chemotherapy more effective?
Preliminary research suggests that strategic fasting may enhance chemotherapy effectiveness by creating differential stress resistance, where healthy cells become more protected while cancer cells become more vulnerable to treatment. However, this approach requires careful medical supervision and may not be appropriate for all patients or cancer types.
What are the risks of fasting for cancer patients, especially regarding malnutrition and weight loss?
Cancer patients face significant risks from fasting, including accelerated weight loss, muscle wasting, weakened immune function, and impaired treatment tolerance. Many patients already struggle with maintaining adequate nutrition due to treatment side effects, making unsupervised fasting potentially dangerous and counterproductive to treatment goals.
How does intermittent fasting affect cancer cell growth and the body's immune response?
Intermittent fasting may influence cancer cell growth by altering metabolic conditions, reducing glucose availability, and enhancing autophagy processes. Some research indicates it could support immune function through cellular renewal mechanisms, but the effects vary significantly based on individual health status, cancer type, and treatment protocols.
Is it safe to try fasting while undergoing cancer therapy, and what precautions should be taken?
Fasting during cancer therapy is not safe without direct medical supervision from oncology healthcare providers. Essential precautions include comprehensive nutritional assessment, regular monitoring of blood markers and body composition, coordination with treatment schedules, and immediate discontinuation if adverse effects occur.
Does fasting reduce the risk of cancer recurrence, and what does the research say about time-restricted eating?
Current research on fasting and cancer recurrence prevention is limited and preliminary. While some studies suggest potential benefits of time-restricted eating patterns for overall health and possibly cancer risk reduction, there is insufficient evidence to recommend fasting specifically for preventing cancer recurrence. More long-term clinical trials are needed to establish safety and efficacy.