Fat necrosis in the breast is a benign (non-cancerous) condition that occurs when fatty tissue becomes damaged and dies. While it can be concerning due to its ability to mimic breast cancer symptoms, understanding this condition is crucial for proper diagnosis and peace of mind. This comprehensive guide explores the key aspects of breast fat necrosis, including its causes, symptoms, diagnosis, and treatment options.
What is Fat Necrosis in the Breast?
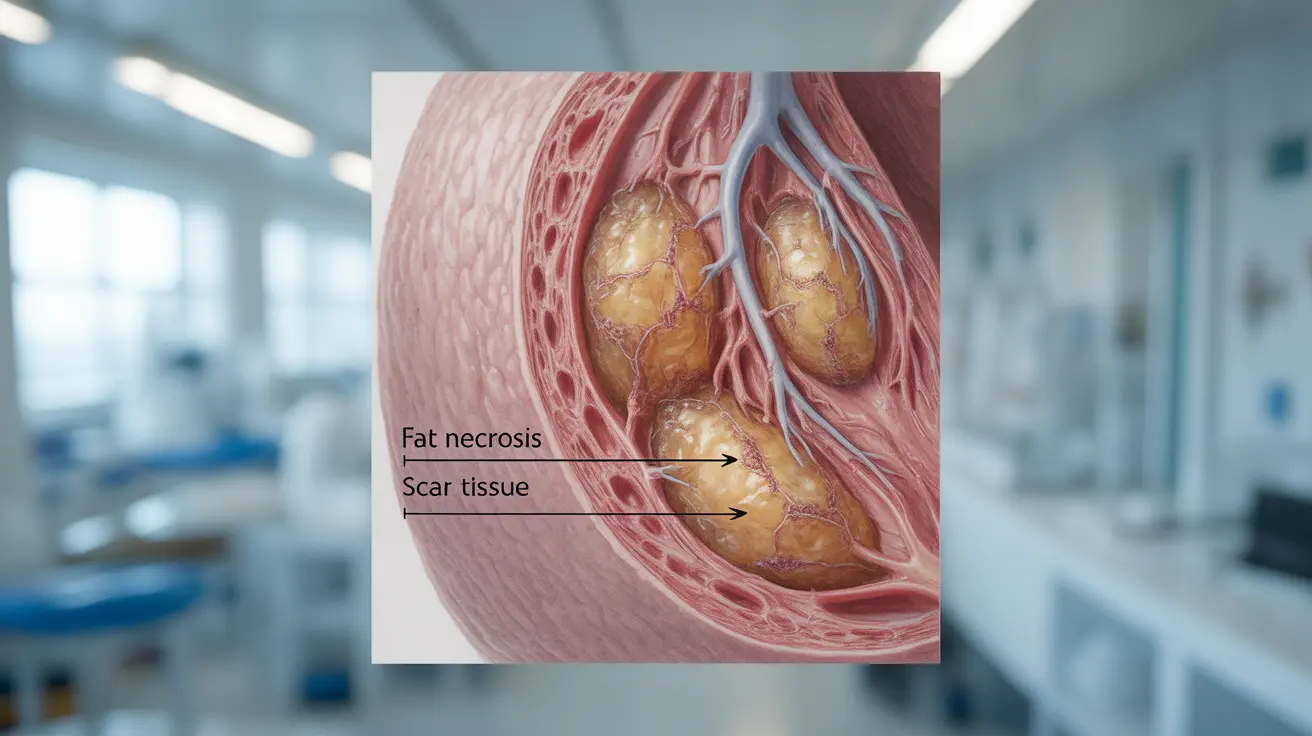
Fat necrosis occurs when breast fatty tissue becomes damaged, leading to the death of fat cells. This damage triggers an inflammatory response in the body, causing the formation of scar tissue. The resulting mass or lump can feel firm and may cause concern, particularly during breast self-examinations.
Common Causes and Risk Factors
Several factors can contribute to the development of breast fat necrosis:
- Previous breast surgery or biopsy
- Radiation therapy to the breast
- Physical trauma to the breast
- Breast reconstruction surgery
- Severe breast injury
Women who have undergone breast cancer treatment or breast surgery are at a higher risk of developing fat necrosis. However, it can occur in anyone who experiences trauma or injury to the breast tissue.
Recognizing the Signs and Symptoms
The symptoms of breast fat necrosis can vary among individuals, but common signs include:
- A firm, painless lump in the breast
- Skin changes or dimpling over the affected area
- Breast tenderness or mild discomfort
- Oil cysts (liquid-filled areas)
- Changes in breast contour
- Skin redness or bruising (in recent cases)
Diagnostic Procedures
Healthcare providers use several methods to diagnose breast fat necrosis and distinguish it from more serious conditions:
Imaging Tests
Common diagnostic tools include:
- Mammogram
- Ultrasound
- MRI (Magnetic Resonance Imaging)
- Digital breast tomosynthesis (3D mammogram)
Physical Examination
A thorough clinical breast examination helps healthcare providers assess the characteristics of the lump and any associated symptoms.
Treatment Options and Management
The treatment approach for breast fat necrosis depends on several factors, including symptom severity and patient preference. Options may include:
Conservative Management
Many cases of fat necrosis resolve on their own and only require monitoring. This approach typically involves:
- Regular follow-up appointments
- Periodic imaging to track changes
- Pain management if needed
Surgical Intervention
Surgery might be recommended when:
- The lump causes significant discomfort
- There's uncertainty about the diagnosis
- The patient prefers removal for peace of mind
- The mass affects breast appearance
Frequently Asked Questions
What are the common symptoms and signs of fat necrosis in the breast?
Fat necrosis typically presents as a firm, painless lump in the breast, often accompanied by skin changes or dimpling. Some patients may experience tenderness or mild discomfort in the affected area.How is fat necrosis of the breast diagnosed and distinguished from breast cancer?
Diagnosis involves a combination of physical examination and imaging tests, including mammograms, ultrasounds, and sometimes MRI. The characteristic appearance on these tests helps differentiate fat necrosis from breast cancer.What causes fat necrosis in the breast, and who is most at risk?
Fat necrosis commonly occurs following breast surgery, radiation therapy, or physical trauma to the breast. Women who have undergone breast cancer treatment or breast surgery are at higher risk, but it can affect anyone who experiences breast injury.How is fat necrosis of the breast treated or managed, and when is surgery necessary?
Many cases can be managed conservatively through monitoring and regular follow-up. Surgery may be necessary if the lump causes discomfort, affects appearance, or if there's diagnostic uncertainty.Can fat necrosis of the breast increase the risk of developing breast cancer?
No, fat necrosis does not increase the risk of developing breast cancer. It is a benign condition, though it's important to continue regular breast cancer screening as recommended by your healthcare provider.