Experiencing nausea or feeling sick after consuming sugar can be concerning, and for many people, it raises questions about diabetes. This common symptom can indeed be related to blood sugar issues, but understanding the connection between sugar consumption, nausea, and diabetes is crucial for proper diagnosis and management.
While feeling ill after eating sugar isn't always indicative of diabetes, it's an important symptom that shouldn't be ignored, especially when accompanied by other warning signs. Let's explore the relationship between sugar consumption, nausea, and diabetes to help you better understand what your body might be telling you.
The Link Between Sugar Consumption and Nausea
When you consume sugar, your body works to process it and maintain proper blood glucose levels. In some cases, rapid changes in blood sugar can trigger nausea and other uncomfortable symptoms. This reaction can occur in both people with and without diabetes, though the underlying mechanisms may differ.
Common Causes of Sugar-Related Nausea
Several factors can contribute to feeling sick after eating sugar:
- Rapid blood sugar fluctuations
- Insulin resistance
- Reactive hypoglycemia
- Delayed gastric emptying
- Underlying digestive conditions
Blood Sugar Levels and Nausea in Diabetes
For people with diabetes, both high blood sugar (hyperglycemia) and low blood sugar (hypoglycemia) can cause nausea. This occurs because extreme blood glucose levels can affect various body systems, including the digestive tract.
Impact of High Blood Sugar
When blood sugar levels rise significantly, it can lead to:
- Dehydration
- Electrolyte imbalances
- Delayed stomach emptying
- Increased acid production
Effects of Low Blood Sugar
Low blood sugar can cause:
- Weakness and shakiness
- Sweating
- Nausea and vomiting
- Confusion
Complications That Can Cause Nausea
Several diabetes-related complications can contribute to feelings of nausea after eating sugar:
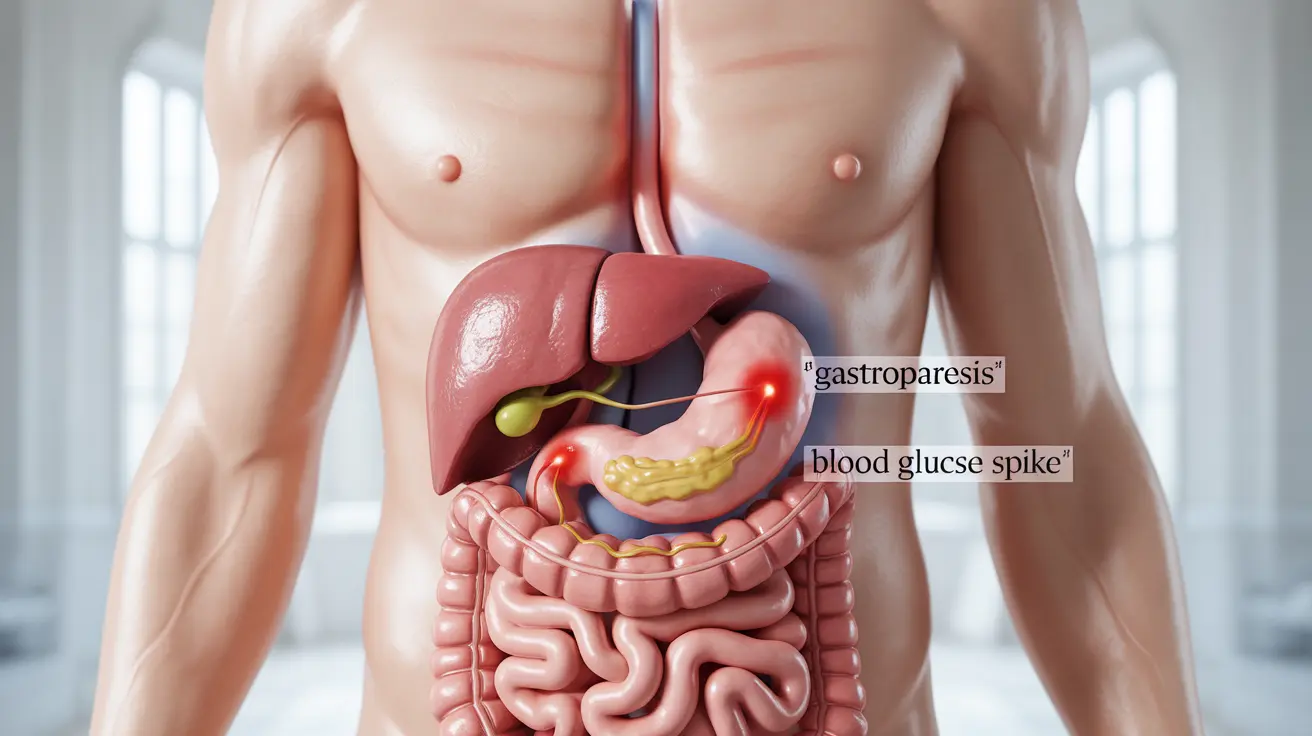
Gastroparesis
This condition occurs when high blood sugar levels damage the vagus nerve, leading to delayed stomach emptying and frequent nausea after meals.
Diabetic Ketoacidosis
This serious complication can cause severe nausea and requires immediate medical attention. Other warning signs include extreme thirst, frequent urination, and breath that smells fruity.
Managing Sugar-Related Nausea
If you frequently experience nausea after eating sugar, consider these management strategies:
- Monitor blood sugar levels regularly
- Eat smaller, more frequent meals
- Choose complex carbohydrates over simple sugars
- Stay well-hydrated
- Work with a healthcare provider to develop an appropriate meal plan
Frequently Asked Questions
Is feeling sick or nauseous after eating sugar a common symptom of diabetes?
Yes, feeling nauseous after eating sugar can be a symptom of diabetes, though it's not exclusive to the condition. This reaction may occur due to rapid blood sugar fluctuations or diabetes-related complications affecting the digestive system.
How do high or low blood sugar levels cause nausea in people with diabetes?
Both high and low blood sugar can trigger nausea through different mechanisms. High blood sugar can lead to dehydration and delayed gastric emptying, while low blood sugar can affect the nervous system and trigger nausea as part of the body's stress response.
Can diabetes-related conditions like gastroparesis cause nausea after meals?
Yes, gastroparesis, a condition where diabetes damages the vagus nerve, can cause significant nausea after meals. This occurs because food moves more slowly through the digestive system, leading to feelings of fullness and nausea.
When should I worry that nausea after eating sugar might be diabetic ketoacidosis?
If nausea is accompanied by excessive thirst, frequent urination, rapid breathing, confusion, or fruity-smelling breath, seek immediate medical attention as these could be signs of diabetic ketoacidosis, a serious complication of diabetes.
What steps can I take to manage or prevent nausea linked to blood sugar fluctuations?
To manage nausea related to blood sugar fluctuations, maintain consistent meal times, monitor blood sugar levels regularly, choose complex carbohydrates over simple sugars, stay hydrated, and work closely with your healthcare provider to optimize your diabetes management plan.