Fluid in the lungs, medically known as pulmonary edema, is a serious condition that requires prompt medical attention. When fluid accumulates in the air sacs of your lungs, it can significantly impact your breathing and overall health. Understanding the signs, causes, and treatment options is crucial for managing this potentially life-threatening condition.
This comprehensive guide will explore everything you need to know about fluid in the lungs, from recognizing early warning signs to understanding treatment approaches and prevention strategies.
Understanding the Condition
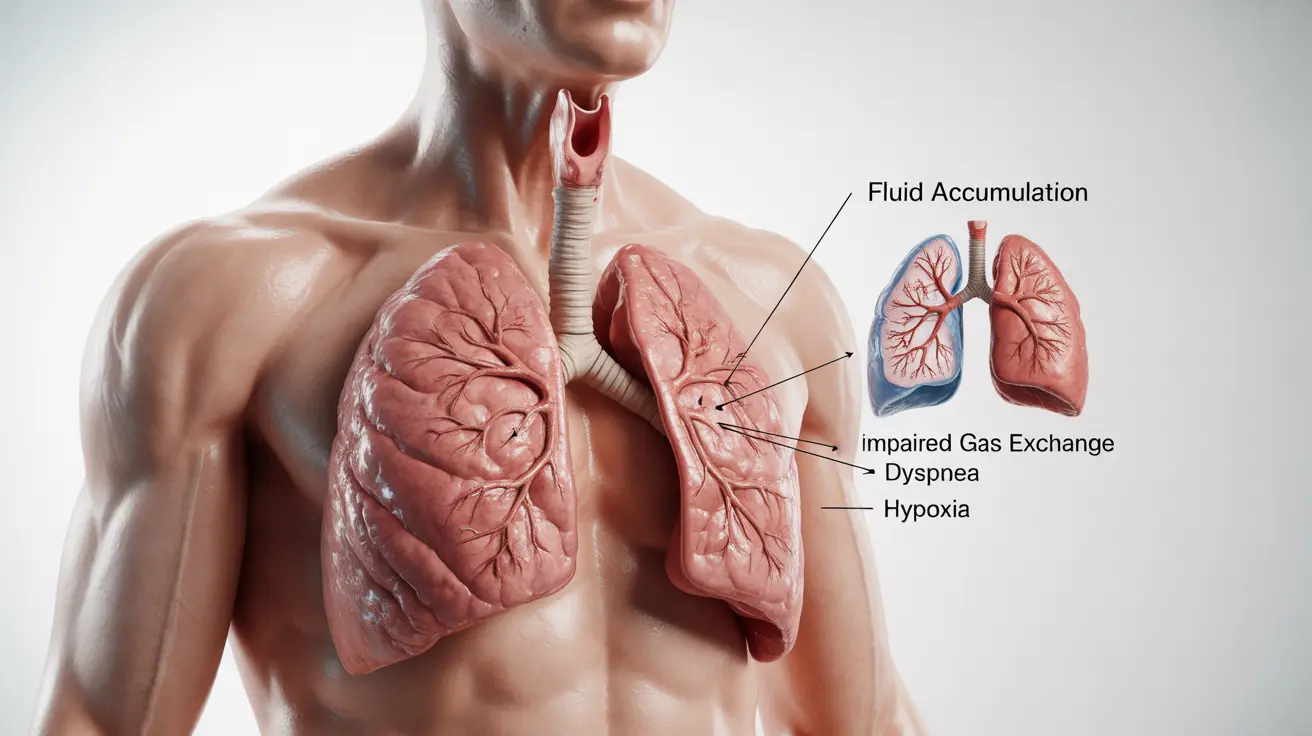
When fluid builds up in the lungs' air sacs (alveoli), it interferes with normal oxygen exchange, making it difficult to breathe. This accumulation can happen gradually or suddenly, depending on the underlying cause. The condition can affect one or both lungs and varies in severity from mild to life-threatening.
Common Symptoms
Recognizing the symptoms of fluid in the lungs is crucial for seeking timely medical care. Common signs include:
- Difficulty breathing or shortness of breath
- Wheezing or crackling sounds when breathing
- Persistent cough, often with pink, frothy sputum
- Rapid, shallow breathing
- Blue-tinted lips or skin
- Excessive sweating
- Anxiety and restlessness
Causes and Risk Factors
Several conditions can lead to fluid accumulation in the lungs:
Cardiac Causes
- Congestive heart failure
- Heart valve problems
- High blood pressure
- Heart attack
Non-cardiac Causes
- Acute respiratory distress syndrome (ARDS)
- Severe infections
- Exposure to certain toxins
- High-altitude exposure
- Kidney disease
- Severe injuries
Diagnosis Methods
Healthcare providers use various tools to diagnose fluid in the lungs:
- Physical examination and medical history
- Chest X-rays
- CT scans
- Blood tests
- Electrocardiogram (ECG)
- Echocardiogram
Treatment Approaches
Treatment for fluid in the lungs depends on the underlying cause and severity. Common interventions include:
Immediate Interventions
- Supplemental oxygen therapy
- Positioning (sitting upright)
- Diuretic medications
- Breathing support devices
Long-term Management
- Treating underlying conditions
- Medication adjustments
- Lifestyle modifications
- Regular medical monitoring
Prevention Strategies
While not all cases can be prevented, certain measures can help reduce risk:
- Managing underlying health conditions
- Following prescribed medication schedules
- Maintaining a heart-healthy lifestyle
- Regular medical check-ups
- Avoiding excessive salt intake
- Quitting smoking
Frequently Asked Questions
What are the common symptoms of fluid in the lungs (pulmonary edema)?
Common symptoms include difficulty breathing, wheezing, persistent cough with pink frothy sputum, rapid breathing, and anxiety. Some people may also experience blue-tinted lips or skin, excessive sweating, and chest pain.
What causes fluid to build up in the lungs and lead to pulmonary edema?
Fluid can build up due to heart problems (such as heart failure or valve issues), severe infections, exposure to toxins, kidney disease, or high-altitude exposure. The most common cause is heart-related conditions that affect the heart's ability to pump effectively.
How is pulmonary edema diagnosed and treated in a medical setting?
Diagnosis typically involves physical examination, chest X-rays, CT scans, and blood tests. Treatment may include oxygen therapy, medications like diuretics, and addressing the underlying cause. Some patients may need breathing support or mechanical ventilation.
What are the emergency signs of pulmonary edema that require immediate medical attention?
Emergency signs include severe difficulty breathing, chest pain, blue lips or fingertips, coughing up pink, frothy sputum, and extreme anxiety or confusion. These symptoms require immediate emergency care.
How can people reduce the risk of developing fluid in the lungs, especially if they have heart or kidney problems?
Risk reduction strategies include following prescribed medication regimens, maintaining regular medical check-ups, controlling blood pressure, limiting salt intake, staying physically active within recommended limits, and managing underlying conditions like heart or kidney disease.