Follicle stimulating hormone (FSH) plays a crucial role in human reproduction and development. This important hormone, produced by the pituitary gland, regulates reproductive function and fertility in both men and women. Understanding FSH is essential for anyone interested in reproductive health or those dealing with fertility concerns.
In this comprehensive guide, we'll explore how FSH works, its significance in fertility, testing procedures, and its applications in reproductive medicine. We'll also examine how FSH levels naturally fluctuate throughout different life stages and medical conditions.
The Role of FSH in Reproductive Health
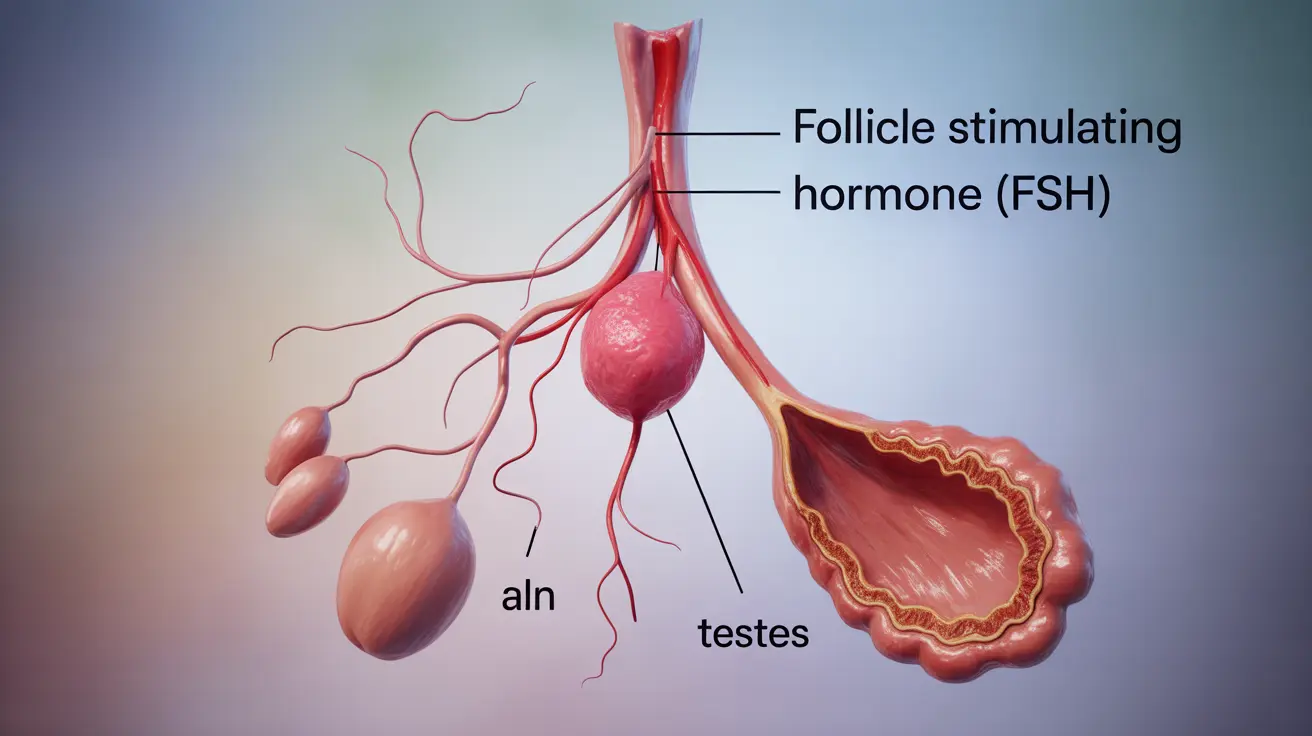
FSH serves distinct but equally important functions in male and female reproductive systems. In women, it stimulates the growth of ovarian follicles, leading to egg development and the production of estrogen. In men, FSH is vital for sperm production, working alongside other hormones to maintain healthy reproductive function.
FSH in Female Reproduction
During a woman's menstrual cycle, FSH levels naturally fluctuate to regulate various reproductive processes:
- Stimulates follicle development in the ovaries
- Promotes estrogen production
- Supports egg maturation
- Helps maintain regular menstrual cycles
FSH in Male Reproduction
In males, FSH contributes to reproductive health by:
- Supporting sperm cell development
- Maintaining sperm production
- Regulating Sertoli cell function
- Contributing to testicular development
FSH Testing and Interpretation
FSH testing is a valuable diagnostic tool for evaluating reproductive health and fertility status. Blood tests measure FSH levels, which can indicate various reproductive conditions or help determine the cause of infertility.
Normal FSH Ranges
FSH levels vary by age, gender, and reproductive stage. Understanding these ranges helps healthcare providers interpret test results accurately:
- Premenopausal women: Varies through menstrual cycle
- Postmenopausal women: Generally higher
- Adult men: Relatively stable
- Children: Lower until puberty
FSH in Fertility Treatment
FSH medications play a significant role in assisted reproductive technologies (ART) and fertility treatments. These treatments can help individuals and couples experiencing fertility challenges achieve pregnancy.
Treatment Applications
Common uses of FSH in fertility treatment include:
- Ovulation induction
- Controlled ovarian stimulation for IVF
- Treatment of certain types of male infertility
- Management of irregular menstrual cycles
Conditions Affecting FSH Levels
Several medical conditions and life stages can impact FSH levels:
- Polycystic ovary syndrome (PCOS)
- Primary ovarian insufficiency
- Hypogonadism
- Pituitary disorders
- Natural aging processes
Frequently Asked Questions
What is follicle stimulating hormone (FSH) and what role does it play in fertility?
FSH is a hormone produced by the pituitary gland that regulates reproductive function. In women, it stimulates egg development and estrogen production, while in men, it supports sperm production. It's essential for fertility in both sexes.
How are FSH levels tested and what do abnormal results mean?
FSH levels are tested through blood samples. Abnormal results can indicate various conditions: high levels might suggest menopause or primary gonadal failure, while low levels could indicate pituitary problems or certain reproductive disorders.
How is FSH used in infertility treatments for women and men?
In fertility treatments, synthetic FSH is used to stimulate ovulation in women and enhance sperm production in men. It's commonly used in IVF procedures and other assisted reproductive technologies.
What are the common side effects or risks of FSH therapy in assisted reproduction?
Common side effects of FSH therapy include injection site reactions, mood changes, and ovarian hyperstimulation syndrome (OHSS). Other potential risks include multiple pregnancies and ovarian enlargement.
Why do FSH levels change during puberty, menopause, or conditions like PCOS?
FSH levels naturally fluctuate during different life stages. They rise during puberty to initiate reproductive function, increase significantly during menopause due to declining ovarian function, and may be abnormal in conditions like PCOS due to hormonal imbalances.