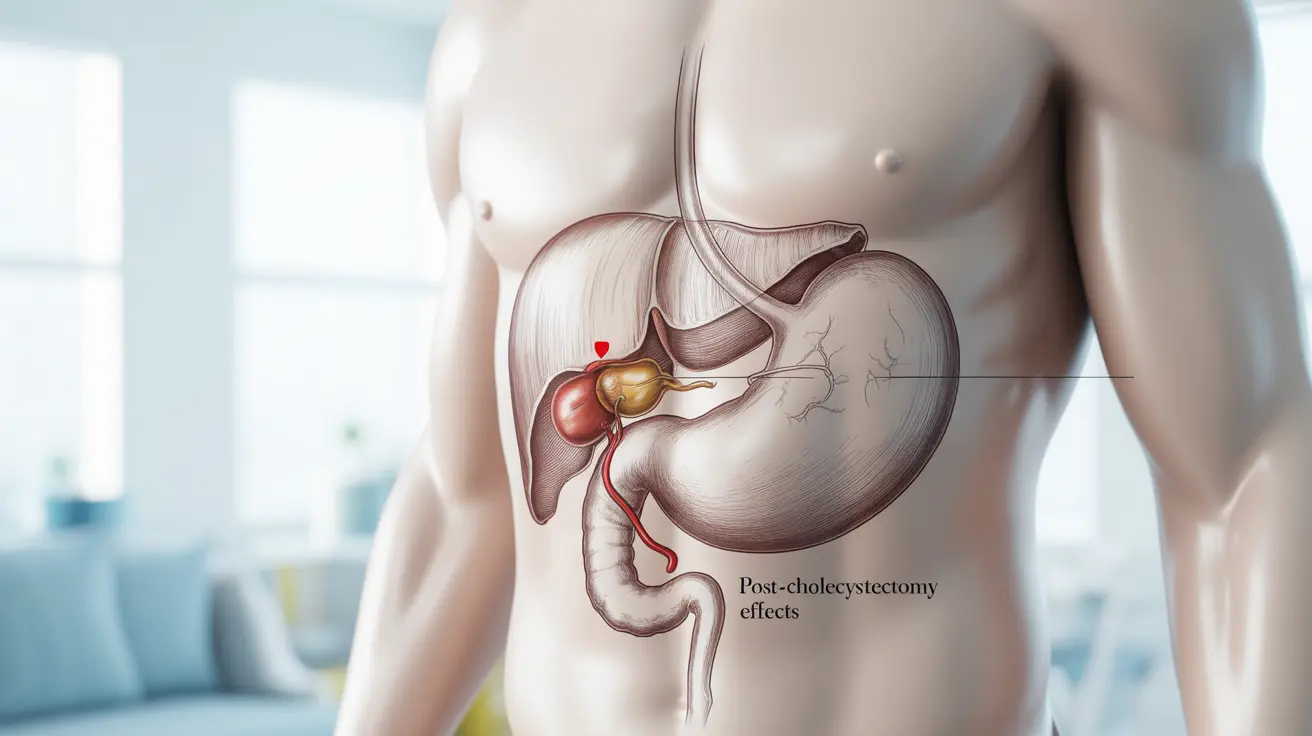
After gallbladder removal surgery (cholecystectomy), experiencing some discomfort is normal. However, persistent or severe gallbladder pain after removal can be concerning and may indicate an underlying issue that requires medical attention. Understanding the causes, symptoms, and treatment options can help you better manage your recovery and know when to seek professional help.
This comprehensive guide explores the various reasons for post-cholecystectomy pain, available treatments, and lifestyle modifications that can help improve your quality of life after gallbladder surgery.
Common Causes of Post-Gallbladder Removal Pain
Several factors can contribute to ongoing pain after gallbladder removal surgery:
Post-Cholecystectomy Syndrome
This condition affects approximately 10-15% of patients who undergo gallbladder removal. It can cause symptoms similar to those experienced before surgery, including sharp abdominal pain, bloating, and digestive issues.
Sphincter of Oddi Dysfunction
The sphincter of Oddi is a muscle valve that controls the flow of bile into the small intestine. After gallbladder removal, this sphincter may become dysfunctional, leading to severe upper abdominal pain and potential complications.
Surgical Complications
Some patients may experience pain due to surgical complications such as bile duct injury, retained gallstones, or adhesions forming around the surgical site.
Diagnosis and Treatment Options
Medical Evaluation
Doctors typically use various diagnostic tools to identify the cause of post-gallbladder removal pain, including:
- Blood tests to check liver function
- Imaging studies (CT scans, MRCP, or HIDA scans)
- Endoscopic procedures to examine the bile ducts
Treatment Approaches
Treatment options vary depending on the underlying cause and may include:
- Medications for pain management and digestive support
- Endoscopic procedures to address bile duct issues
- Dietary modifications and lifestyle changes
- In some cases, additional surgical intervention
Lifestyle Changes for Pain Management
Making certain lifestyle adjustments can significantly improve symptoms:
Dietary Modifications
- Eating smaller, more frequent meals
- Reducing fat intake gradually
- Avoiding trigger foods
- Staying well-hydrated
Physical Activity
Regular, moderate exercise can help improve digestion and reduce post-surgical complications. Start slowly and gradually increase activity levels as approved by your healthcare provider.
When to Seek Medical Attention
Contact your healthcare provider immediately if you experience:
- Severe, persistent abdominal pain
- Fever or chills
- Yellowing of the skin or eyes
- Persistent nausea or vomiting
- Dark urine or light-colored stools
Frequently Asked Questions
What causes stabbing pain after gallbladder removal surgery?
Stabbing pain after gallbladder removal can be caused by post-cholecystectomy syndrome, sphincter of Oddi dysfunction, surgical complications, or adhesions. The exact cause needs to be determined through proper medical evaluation.
How can post-cholecystectomy syndrome be diagnosed and treated?
Diagnosis typically involves blood tests, imaging studies, and possibly endoscopic procedures. Treatment may include medications, dietary changes, and in some cases, endoscopic or surgical interventions.
When should I see a doctor for pain after having my gallbladder removed?
Seek immediate medical attention if you experience severe persistent pain, fever, jaundice, prolonged nausea or vomiting, or significant changes in bowel habits.
What lifestyle changes can help reduce pain and digestive problems after gallbladder removal?
Key lifestyle changes include eating smaller, more frequent meals, gradually increasing fat intake, avoiding trigger foods, staying hydrated, and maintaining regular physical activity as approved by your healthcare provider.
Can sphincter of Oddi dysfunction cause severe pain after gallbladder surgery and how is it managed?
Yes, sphincter of Oddi dysfunction can cause severe upper abdominal pain after gallbladder removal. Management typically includes medications, dietary modifications, and sometimes endoscopic procedures to address the dysfunction.